These drugs are quite expensive. But, are they worth it?
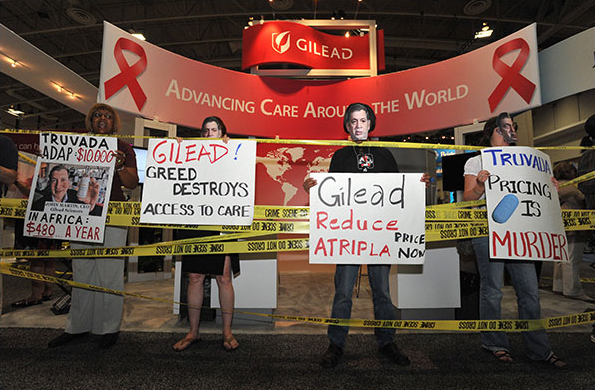
The fallout from the pricing of these drugs was inevitable, and closely mirrors what happened with HIV/AIDS about 15 years ago. Following a massive ten year campaign, which included contributions from virtually every major pharmaceutical company, drugs that could stop or slow the replication of HIV (and extend the life of HIV-positive patients) became available. These drugs were also expensive, and AIDS activist group showed their displeasure by, among other things, chaining themselves to the fences surrounding the homes of the CEOs of some of the companies that were selling the drugs.
I am not aware of any fence chaining, but criticism of the price of HCV drugs—especially Gliead's Sovaldi, which costs $1,000 per pill—is fierce. In fact, the May 7th Medscape daily email entitled "Hepatitis C: Cure, but at what cost?" featured nine articles about the high cost, including "Costs to Public of USD 84,000 Hep C Drug 'Outrageous,' and "WHO Joins Clamor to Make New Hepatitis C Pills Affordable."
So, are these new drugs too expensive? I guess that depends on whether you're buying or selling them. But, in order to determine the actual value of something like Sovaldi, you have to look at what it replaced—a therapy that was very difficult to tolerate, only modestly effective, and also rather expensive.
The standard of care for hepatitis C only two years ago was a combination of interferon and ribavirin, and it was god awful—mostly due to the interferon. In his blog, "Antibiotics-the Perfect Storm," Dr. David Shlaes, the former head of infectious disease research at Wyeth elaborates: "Before Gilead’s Sovadi, the standard treatment was 24 – 52 weeks of interferon plus ribavirin. Interferon causes fever, chills, depression, low blood counts and a number of other problems. It has to be administered by intravenous injection monthly. Other drugs have to be used to counteract its side effects. Ribavirin is given as a pill (many pills) and causes anemia among other things. Sometimes transfusions are required to maintain blood counts throughout a course of therapy. And after you have finished the entire course, the failure rate of this therapy can be as high as 50%."
And let's not forget the costs of not using Sovaldi. A course of Interferon plus ribavirin costs $30,000. A liver transplant will set you back more than $500,000. And the anti-rejection drugs needed after the transplant cost $20,000 for the first year following transplantation.
All of a sudden the 84K doesn't seem so bad, does it? And Sovaldi is the only interferon-free therapy that is approved by the FDA for treatment of hepatitis C. The first generation HCV protease inhibitors, Incivek (Vertex) and Virtrelis (Schering/Merck) significantly improved the cure rate, but these were only approved for use in combination with interferon—not in place of it.Other companies, notably AbbieVie, whose ABT-450 is expected to gain FDA approval soon, are studying interferon-free HCV drug combinations. These drugs will also be expensive.
But as Dr. David Berstein, chief of hepatology at the Center for Liver Disease, North Shore University Hospital, Manhasset, New York, and co-author of a paper in the May 4th New England Journal of Medicine said in a recent interview, “We in this country look at cost, because it costs a lot. But you are curing 97% percent of patients in 12 weeks–so, what is the value of that?”
This is no time to fool around. These drugs have the potential to wipe out hepatitis C, which has infected three million Americans, and 170 million people worldwide—about four times that of HIV.
No- new hepatitis C drugs are not too expensive. They are appropriately expensive. Advances like this come up once in a lifetime. The companies that devoted many years and spent billions of dollars to make this happen should be rewarded. And when you factor in the high cost and high failure rate of the previous treatment, this actually becomes a bargain.




Comments