In some cases, I agreed with them. They were thirty years old, weighed 400 pounds and had a medication list like a nursing home patient. Those guys, I worried about. But many of my weight management patients were 50-100 pounds overweight at age 50 and on just a couple medicines.
For an overweight or moderately obese person, what’s the real risk? What would be the real benefit of weight loss, in terms of number of years on the planet?
One answer comes from the work of H. Gilbert Welch and Steven Woloshin, who frequently challenge the common wisdom on medical issues. In a 2008 paper from the Journal of the National Cancer Institute, they assess the absolute risk of death for U.S. adults at various ages. It shows, among other things, just how resilient we diseased, obese, Americans really are. Taking their raw survival numbers and placing them in a simple graph form shows:
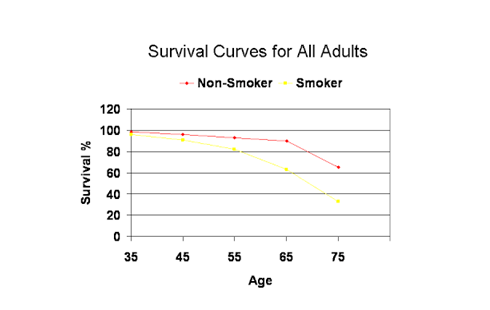
What this chart depicts is the ten year survival, for men, at different ages. For example, if you’re 35 and not a smoker, you have a 98.5% chance of making it to 45. At 45, you would re-calibrate with those that are still alive and there is a 96% chance of living ten more years, then 93% for the next ten, then 90% for the next. Finally, at age 75, life gets a little risky and the chance that you will live another ten years drops to only 65%. Essentially, the ten year risk of death is almost negligible until we get to our 70s.
Notice that the only group that needs to be separated out as having remarkably different risk is smokers. This lifestyle choice is so dangerous that you can’t talk about longevity in smokers and non-smokers together. More importantly, for my perspective, is that blood pressure, cholesterol, weight, blood sugar, all those risks we worry so much about, are nowhere to be seen. This is not because they weren't assessed for this study, they simply don't matter enough to change the statistics.
This is all comers. Everyone who lives in the U.S. Well and unwell. Skinny and chubby. Drinkers and non-drinkers. This is everyone. Everyone has, at age 55 (if they’ve made it to age 55) a 93% chance of living ten more years! And if you are consciously trying to make good choices (not riding a motorcycle, not playing with handguns near your in-ground pool while intoxicated) you probably are almost certain to live ten more years.
What would you expect to find if you looked harder for correlations between body mass and death statistics? I think most of us feel that being heavy is a pretty serious risk factor for death, since increased weight is associated with diabetes, heart disease and a long list of other ailments. Most doctors would probably assume that as you move from a normal body mass index of 18.5-25, to an “overweight” BMI of 25-30 and “obese” BMI of greater than 30, that the risk of death would climb in a pretty linear fashion. The heavier you are, the worse off you are.
But that's simply not true.
In a 2011 paper published in the New England Journal, Zheng and colleagues looked at health records and death statistics for over one million people over the course of 9 years. What they found is that being obese (BMI greater than 30) was associated with an increased risk of death for East Asians, but not Indians or Bangladeshis. They also found being significantly underweight (BMI less than 20) was associated with increased risk of death. But in between these two categories (weights from 130-190 if you’re 5, 7”) the risk was flat. There was no difference in longevity for a range of body weights fluctuating 60 pounds or so.
This type of relationship, where you measure one variable against another and the extremes seem to correlate with the outcome you’re interested in, is called “U-Shaped,” since the lowest correlation is right in the middle. For weight, this is pretty logical: if you’re very underweight, you are likely starving, frail, or ill already, so that’s higher risk for death. If you’re very obese, you tend to be unwell too, so no surprise there. But the “U” in the data by Dr. Zheng, et al, was surprising, in that the bottom was essentially flat between 20 and 30 BMI. The data seemed to suggest that being BMI 30 is no less healthy than a BMI of 20 in this population. And the Indian group and Bangledeshi group showed no increased risk at all for the higher BMIs. One wonders whether some of the correlation may have been lost due to the authors grouping all BMIs greater than 32.6 together. (Presumably this reflects that Asian populations have fewer people in the higher categories than are typically reported in North American populations).
The New England Journal is not unique in finding that BMIs 20-30 seem to share equal mortality risk. In a paper more about data analysis than the findings themselves, Drs H. Gilbert Welch, Schwartz and Woloshin looked at what they called “The exaggerated relations between, diet, body weight and mortality.” They demonstrated that the drawing of the “U-shaped” curve smooths out a lot of differences in the BMI groups and averages out differences between groups to make this relationship look linear when it’s not. In terms of risk of mortality, the authors showed that bar graphs (and categorical analysis) represented the data better than a curve and made it much more obvious that little difference exists between BMIs of 20-30.
In “BMI and Mortality: Results from a National Longitudinal Study of Canadian Adults” Heather Orpana, et al, found in a sample population of ~11,000, that the “overweight” group was at significantly decreased risk of death, a bit more so than what was found in these other two studies. They also found the individuals classified as obesity class I (BMI 30-35), were at no increased risk for death.
This same finding, that BMI between 20-35 contain no difference in risk and that the lowest death rate was for BMI 27, was produced in two separate papers by Katherine Flegal, in 2005 and again in 2013. Both papers were extremely carefully done and published in JAMA. This lower risk of obesity for overall mortality has been shown so many times that we need to stop considering it a surprise and realize, again, that we aren't thinking clearly about what obesity actually is.
Obesity is not some disease state that causes early death, but a physical sign that runs with other signs and symptoms, because it is a product of the modern way of living, just as hypertension and high cholesterol are the products of modernity. It doesn't actually cause any outcomes at all.
The most feared outcome we generally link to obesity is early cardiac death. In 2011, Canto and colleagues published in JAMA, a study that looked at a cross-sectional view of heart attack patients from 1994-2006 in U.S. hospitals. The researchers’ interest was in determining how patients fared based on whether they had various risk factors, such as: hypertension, smoking, high cholesterol, diabetes or family history of heart disease. The surprising conclusion was that the fewer the number of risk factors a patient had at the time of the first heart attack, the worse they did. The researchers found that if you have a first heart attack and you are a non-smoker, non-diabetic with normal blood pressure, good cholesterol and no family history, you are more likely to die than someone who has all of those things.
But that’s not the interesting part. At least not to me. The interesting part is the raw numbers that they examined from National Registry of Myocardial Infarction. What the straight numbers mostly show is that the group of patients you might find on any given day in the cardiac ward of a hospital looks pretty much like the general population:
52 % have high blood pressure
28 % have high cholesterol
22 % have diabetes
31 % smoke
28 % have a family history for heart disease
This is for a group of people with an average age of 66. Those numbers, aside from the smoking, (which would have been even higher if they included former smokers) basically reflect the going rates of those factors in adults in that age group. The same is true for the breakdown on obesity:
28 % were normal weight (BMI 18-25)
36 % were overweight (BMI 25-30)
32 % were obese (BMI >30)
Which is essentially the same as what you’d get walking down most U.S. streets taking a random sample of adults.
So what does this mean for how we think about risk?
We tend to over-estimate how dangerous an individual risk factor is. We don’t have good statistical brains, so we try to make meaning out of things using logic rather than numbers. "Cholesterol gives you a heart attack,” makes more sense to our logic-craving brains, than “high cholesterol significantly increases risk for a heart attack in some people.” We certainly aren’t good at keeping track of whether relationships hold going both forward and backward. For instance, thinking that high cholesterol causes heart attacks lends itself to the conclusion that all or most heart attack patients must have high cholesterol. But in this sample, 72% of the patients with a first heart attack had normal cholesterol. Let’s invert the rest of the factors, as well:
48 % did not have hypertension
78 % did not have diabetes
69 % were non-smokers
72 % had no family history for heart disease
64 % were not obese
How would those numbers look on a public health poster or a billboard? It’s hard to scare people into doing what you want, like being screened, or joining your lifestyle program, if you can’t find the lifestyle factor to blame:
“78% of all heart attack victims have normal blood sugar. Be tested to ensure you don’t have normal blood sugar."
The surprise in these numbers comes back to the difficulty of separating out, in our day to day thinking, the difference between absolute risk and relative risk. A clear example of this is the fact that Celebrex cuts your chance of having a bleeding ulcer in half compared to ibuprofen (relative risk). The fact that it’s cutting it from 3% to 1.5% (the absolute risk) is not something that the promoters of the safer medicine spend much time on, because, who (an individual or an insurance company) would be willing to spend 25 times more for a medicine that prevents a problem from occurring almost never to…a little less than almost never?
Bleeding ulcers give interesting absolute numbers because they are rarer than you might think. Our brains want a simple rule like, “take a lot of ibuprofen, you’ll get a bleeding ulcer.” But in fact, you’re statistically unlikely to get a bleeding ulcer, even with the ibuprofen (97% chance of not having a bleeding ulcer) because they are fairly rare. Our brain can’t do much with, “take a lot of ibuprofen and it’s still much more likely than not that your stomach is fine.” That just doesn’t compute.
The heart attack numbers are surprising for the opposite reason: heart attacks are so common that finding the one, absolute, cause is unlikely. For a heart attack, the true statement is “you can have one even if you do everything right.” We can debate whether novice runners having signs of heart damage from marathons is good or bad for them, but the fact that running legends like Jim Fixx and Alberto Salazar had heart attacks is due to probability. Lots of people have heart attacks, some are elite runners. Marathon runners having heart attacks remains surprising for the right reason: good fitness is protective for the heart.
In the JAMA study, 86 % of the heart attack patients had at least one factor that put them at increased risk. However, the risks are common in all people, so it would be difficult to find 60 year olds without these. The breakdown looked like this:
0 risks: 14 %
1 risk: 34 %
2 risks: 32 %
3 risks: 15 %
4 risks: 4 %
5 risks: 0.4 %
Again, the risks run almost exactly opposite of our knee-jerk expectations because we aren’t good at remembering that it gets statistically unlikely to have multiple probabilities occuring in the same person. Looking at combined probability, remember, involves multiplying decimals by other decimals, so numbers shrink quickly. The only reason the above numbers are as high as they are, is because these risks are not independent factors, but very interdependent: they run together.
This study isn’t about what causes heart attacks. There have been many of those studies and they show exactly what you’d expect: there is a linear rise in risk for heart attack as one becomes heavier, has higher blood pressure, smokes longer, etc…This study isn’t questioning that. However it does show that much of the risk of a heart attack (the most dreaded outcome of all these metabolic risks we try to control by weight loss) is not subject to our control. The doctors and purveyors of tests (talking about myself here) who claim they can predict and reduce risk for dreaded outcomes are focused on individual factors that simply aren't that important for most individuals. Close to half of the cases in the heart attack registry would seem like random tragedies, not controllable or preventable through diet, exercise or reducing risk factors with medication. What’s strange is how well these sick people would have looked the day before their heart attack.
Why I find this interesting, in the context of our ongoing discussion of obesity and how much it matters for health, is that we can’t control a lot of the risk that’s out there. We want to lose weight to avoid a heart attack, but the effect weight loss has on decreasing risk of heart attack has never actually been studied. We have an assumption that most people who have a heart attack have a weight problem, but that simply isn't true; the heart attack victims have the same rate of obesity as the general population. Chance and other factors outside of our control likely have more power over our future disease risk, even in the category of lifestyle diseases, than we do ourselves.
We want there to be answers, that is our make up. That is the story of human progress: modern man faces mysteries and problems, scientists uncover the laws that govern the mystery, man's technology uses this knowledge to provide a solution. This does happen, but it has not happened in any field dealing with diet.
An oft repeated concept, when you are in medical school is that "one half of what you learn here will later be proved to be false...we just don't know which half yet." It's a catchy idea, but most likely mis-applied. The vast majority of the time in medical school is spent in the lecture hall, learning basic science that doesn't change. Where we are taught false ideas is most certainly out on the wards, when the experienced physicians show us treatment algorithms for diagnosing and treating serious ailments. At a stretch, it is possible to conceive of 20-30% of those strategies being discarded for improved methods over a few decades, but the idea that half of what is taught is inaccurate seems silly and un-testable to me.
Nevertheless, on the treatment side, how much of what we do is actually necessary? How helpful is modern medicine?
It's a deeply held belief that physicians and the medical industry do people a world of good. We believe that as we grow older, the regular visits to the doctor will keep us healthy. She will screen us for cancers, check our cholesterol, measure our blood pressure, adjust our medicines and this will keep us alive a decade longer that we otherwise would have lived, say, a century ago. This is part of the national ethos. Primary care doctors prevent heart attacks and cancers by treating the risks and catching diseases before they can harm us. For some diseases, like preventing strokes by lowering blood pressure, this may be true. But for many others, we do not have data that show our treatment helps, or that it helps to the extent that the patient and doctor believe.
This is important to the current treatment approach to weight problems because the underlying assumption is that if we can describe obesity as a medical illness, unravel the biological pathology, this will lead to medicines to "cure" it. I think that this is wishful thinking for a number of reasons, the most important of which is the complexity of regulation that I have been writing about in these posts. But if we could "cure" obesity using as-yet-only-dreamed-of medications that help to lose weight, what would the real gain be? As we've just discussed, heart attack victims weigh the same as the general population and the papers on mortality show that obesity is not associated with early death except at the very extreme. How could these magical weight loss pills really improve our health? Should we just turn our attention elsewhere?




Comments