Sample Radiation Protection and Safety/ALARA Program based on Philippine Perspective
Statement from the management.
I. Organization and Responsibilities
Chair
Vice-Chair
Board members
Personnel
Authorized user
Radiation protection officer
Supervisor
Medical physicist
Radiation therapist
Moulding technologist
Radiation oncology nurse
Duties and Responsibilities
A. Radiation Protection Committee/Medical Isotope Committee
The main duty of the Radiation Protection Committee is to establish a radiation protection policy according to BHDT and PNRI and the specific requirements contained in the installation’s license to possess and use radiation sources. It also should be the link between the Radiation Oncology Facility and the Regulatory Authorities.
Other ResponsibilitiesB. Radiation protection officer (RPO)
• Review the potential hazards arising from the use of ionizing radiation with respect to diagnosis, therapy and research, with a view of ensuring adequate standards of protection for patients, staff and the general public.
• Review and oversee compliance with, and implementation of, the (As Low As Reasonably Achievable) ALARA program.
• Formulate radiation protection policies to update and improve the Radiation Protection Programme/ALARA program.
• Investigate any radiation incidents or accidents and provide a comprehensive report on these to the employer and regulatory authorities.
• Assess potential hazards from foreseeable incidents and prepare contingency plans.
• Correct identified deficiencies in the ALARA program.
• Review new uses of radiation sources that may lead to modifications of the ALARA program.
• Identify any amendments to the license.
• Identify staff needing personal authorizations.
• Ensure that radiation equipment, sources, shielding procedures and safety standards satisfy such specific requirements and/or recommendations as may be issued from time to time by the regulatory agencies; and to ensure that the appropriate organizational arrangements exist for compliance with such requirements and recommendations.
• Oversee the use of licensed radiation sources and operation of radiation equipment throughout the institution’s radiation safety program.
• Familiar with all pertinent Bureau of Health Devices and Technology (BHDT) and PNRI regulations.
• Review, and to approve or disapprove the use of radiation sources and generators in the radiation oncology center, from the standpoint of radiation safety; to authorize the acquisition of these materials through the license holder, where necessary, to apply additional conditions to such use, other than those stated in the relevant license; and to suspend such use where appropriate.
• Review, and approve or disapprove from the standpoint of radiation safety, requests for the acquisition, installation and housing of equipment capable of producing ionizing radiation.
• Approve designs of rooms to be utilized for treatment and diagnosis.
• Ensure that adequate system of radiation monitoring is undertaken in all sections in which ionizing radiation is employed, and to review quarterly RPO’s summary report of occupation radiation exposure records of all personnel giving attention to individuals or group of workers whose occupational exposure appears excessive.
• Ensure that plans are prepared, and suitable equipment made available to deal with accidents and emergencies involving an actual or potential radiation hazard.
• Review the training and experience of the proposed authorized users, RPO, and radiation workers and to determine that their qualifications are sufficient to enable the individuals to perform their duties safely.
• Meet as often as necessary but not less than once in each calendar quarter. To maintain written minutes of all convocations.
• Review the RPO’s summary report of the entire radiation safety program at least annually and recommend remedial action to correct any deficiencies identified in the radiation safety program.
• Establish a program to ensure that all person whose duties may require them to work in areas where ionizing radiation is used, e.g. nurse, security, housekeeping, etc. are appropriately instructed.
• Ensure that licenses to operate machines utilizing ionizing radiation sources are amended if required, prior to any changes in facilities, equipment, policies, procedures and personnel.
• Evaluate the activities of the Radiation and Health Safety Officer in implementing the various measures laid down in this document.
• Establish program for the maintenance of reports, records, and actions.
• Review quarterly the summary of the occupational radiation dose exposure records of all personnel working with radiation and records of radiation level survey.
• Review quarterly, all incidents involving radiation with respect to cause and subsequent action taken.
• Ensure the effective implementation of facility's Radiation Safety Programme (ALARA) is in compliance with the applicable Sections and Parts of DOH-BHDT and PNRI regulations.C. Radiation Workers
• Perform an annual review of the radiation safety program in adherence to ALARA concepts.
• Assess and evaluate the occupational exposures of authorized users and workers on a quarterly basis in accordance with established values of effective dose limits and levels of investigations set and agreed upon by the organization.
• Schedule briefings and education sessions to inform workers of ALARA program efforts.
• Establish procedures for receiving and evaluating suggestions of individual workers to improve the current health practices.
• Investigate all known instances of deviation from good ALARA practices and determine the causes in order to introduce appropriate modification in the program to maintain exposures ALARA.
• Communicate with DOH-BHDT as often as necessary to respond t inspection findings and requests for renewal or amendment of license or to seek clarification regarding regulatory commitments and other information.
• Develop a mechanism to ensure continuity of radiation safety of staff.
• Establish, maintain and audit written policies and procedures to implement various aspects of the radiation safety program.
• Ensure that radiation safety issues are addressed in a comprehensive and timely manner, audits are conducted as required, feedback mechanisms are in place to correct deficiencies and that adequate resource are provided to implement the radiation safety program or when modifications are needed.
• Participate in the early planning stages of designing new or remodeling existing facilities that will be used for patient procedures involving ionizing radiation.
• Initiate investigations into possible over exposures from radiation accidents.
• Ensure that the required radiation protection surveys are regularly conducted with license commitments and regulatory commitments.
c1. Authorized Users
An authorized user is a person who is officially designated, for licensing or other purposes, as the individual responsible for the procurement and use of specified radiation sources. He/she is responsible for supplying the facility and supervision needed by the staff. The authorized user shall have the following functions:c2. Radiological Supervisor
• Coordinate with RPO/Medical physicist the planning stage regarding the safety aspects of new procedures involving potential radiation exposures.
• Evaluate all procedures before using ionizing radiation sources to ensure that exposures will be kept ALARA.
• Ensure that the workers under his/her supervision are trained and educated in good health physics practices.
• Responsible for the safe use of licensed materials in humans by prescribing correct radiation dose to be administered to the patient for treatment.
• Responsive to the concerns of the RPO regarding the regulatory commitments and safe practices, or any relevant issues.
• Checks daily endorsement prepared by staff of each section.c3. Medical Radiation Physicist/s
• Performs daily rounds and check the activities of each section.
• Prepare the necessary documents for the renewal of license to operate radiological facilities.
• Supervises Radiologic Technologist in their administrative functions.
• Attends administrative meetings.
• Prepares management reports/communications when indicated.
• Check and approves sections schedule.
• Directly supervises all activities of radiotherapy technologists.c3. Radiation Therapists
• Acceptance testing of Radiotherapy equipment.
• Routine Calibration of Radiotherapy equipment.
• Development of a quality control program and carrying out tests to reassure efficient and reliable performance of equipment.
• Collaborate with the Radiation Oncologist and Radiation Therapists in the treatment planning verification and execution of plans.
• Calculation of dose distribution in and around tumor and surrounding normal tissue.
• Ensure correct radiation dosimetry in external beam teletheraphy.
• Design of auxilliary devices neede for accurate treatment of patients.
• Performance of after repair tests of radiotherapy equipment in collaboration
with the maintenance engineer.
• Give lectures to medical oncologist, radiation therapists and nurses on radiation physics, protection, and dosimetry.
• Provide physics support to research.
• Conduct training sessions on radiation safety issues for radiation technologists
and/or other health care professionals. This shall include:
a. Basic Radiation Physics
b. Radiation Detection and Measurement
c. Radiation Monitoring and Area Monitoring
d. Emergency Preparedness and Response
e. Handling of Radiation Therapy Patients
f. Radiation Therapy Procedures and Techniques
g. Quality Control in Radiation Therapy
h. Licensing Rules and Regulations
i. ALARA Program
The Chief Radiation Therapist shall:
• Supervise staffs and teaches Radiotherapy trainees.The Radiation Therapists shall:
• Assist Radiation Oncologist and Medical Physicist during patient set-up, treatment planning and treatment.
• Supervise the performance of RT in their technical function.
• Maintain section records, inventories, supplies and equipment.
• Perform all the examinations/treatment as requested.
• Report directly to the supervisor any problem encountered within the section.
• Submit recommendation to the supervisor regarding staff performance evaluation.
• To discuss the problem and to come up with suggestion/solution to the problem and to inform what is going on in area of responsibility to the department head and supervisor.
• Prepares material for treatment (planning and simulation). Set-up machine for tumor/target localization, take radiograph of tumor site.
• Give instruction and explain the preparation required for corresponding procedures.
• Give lectures and assist in technological training of medical and paramedical courses.
• Do monthly such as: Income proof, statistic report, consumption, referrals.
• Ensure that patients receiving radiation treatment understand the importance of treatment procedures.c4. Moulding Technologist
• Cautiously and carefully position the patient such that the useful radiation beam is directed and limited to the anatomical area to be treated.
• Double check all treatment parameters before setting the treatment timer/monitor unit setting according to the prescribed treatment dose.
• Apply appropriate shielding blocks, wedge filters and other accessories as prescribed in the treatment plan whenever necessary to achieve high accuracy of dose distribution within the volume of interest.
• Perform and document the results of many routine tasks for the safe use of licensed material as established in the radiation safety program.
• Assist the authorized users and medical physicist in ensuring that the treatment portal or location is accurate and that all instructions and information regarding administration of prescribed dose are clearly recorded and understood by all responsible parties.
• Ensure that the fractionated dose is administered as prescribed each time on a daily basis and that the correct patient receives the appropriate prescribed dose.
• Maintain required records to document safety checks and procedures, and various other aspects of the radiation safety program.
• Always be alert and prepared for any radiation emergency incidents or accidents that may arise during the course of the radiation therapy procedures.
• Assist the medical physicist in the calibration, quality control and maintenance of the teletherapy machine.
• Inform the RPO of any abnormal incidents that may occur in the radiotherapy facility.
• Clean Linear Accelerator machine, Simulator machine and other equipment’s machine, keeps all rooms accessories in order.
• Give lectures and assist in technological training of medical an paramedical courses.
• Implement Oncologist and Medical Physicist order.
• Assists the medical physicist in taking the radiograph of the tumor site.c5. Radiation Oncology Nurse
• Prepares the necessary material for making blocks.
• Prepares the mould blocks for patients based on the simulation film in accordance with established procedures and puts labels indicating the patient’s name.
• Maintain/records patients whose blocks have already been prepared.
• Ensures timely moulding of blocks have already been prepared.
• Ensures timely moulding of blocks to be utilized by patients during treatment.
• Maintains and updates record of material consumption used in the preparation of blocks such as Styrofoam,cerrobend, moulding tray, cutting wire and mounting tray.
• Ensures the cleanliness and proper functioning equipment and after care of styrocutter.
• Maintains close coordination with the Chief Radiation Therapist in case of equipment malfunction.
• Helps the Radiotherapist in the preparation of the patient.
• Assist in transporting of patients to the treatment room.
• Performs other tasks that maybe assigned by immediate superior from time to time.
• Assist doctors during check-up and evaluation of cancer patients such as internal examination, etc.II. Workplace Monitoring, Area Classification and Individual Monitoring
• Dress and clean wounds and open lesions of cancer patients.
• Ask patients to sign consent form for treatment.
• Check the weight (in pounds) and blood pressure of the patients.
A. Workplace Monitoring
Periodically, the equivalent dose rate shall be measured at the door, and control console and physics rooms during BEAM ON. Dose rate at these rooms and at the level of the door should be limited to 1 μSv/h. Dose rate reading in excess must be noted by the RPO and determine possible causes such as machine breakdown or loss of shielding capacities of barriers.
B. Controlled and Supervised Areas
The designation of an area as controlled will mean that nobody will be allowed to enter the area unless subject to a system of work. In our facility, the room where radiotherapy equipment is used is classified as CONTROLLED AREA. It is stressed that in no circumstance that any person other than the patient is allowed during “BEAM ON.” The rooms adjacent to the treatment room where regular radiation work is carried out shall be classified as SUPERVISED AREA. These are the Control/Console and Physics Rooms. The dose constraints (effective dose rates) at the supervised areas will be 1 μSv/h. Areas which do not require official designation because the doses which personnel are likely to receive are less than 1 μSv/h are referred to as non-designated areas. Other areas other than the control and supervised areas will have a dose constraint of 0.02 mSv/wk.
C. Personnel Monitoring and Protection Program
Personnel monitoring device such as a thermoluminecent device (TLD) shall be supplied to all individuals occupationally exposed to ionizing radiation. A personnel monitoring device is also called a personal radiation monitor. The monitor must be worn by the same person for the duration of the monitoring period, hence the word “personal.” All physicians, medical physicist, radiation therapist, aides assigned to the Linear accelerator shall be issued with TLD badges. These badges will come from the PNRI and will be processed thereby a contract service on a monthly basis. The following shall be observed:
• Individuals occupationally exposed to radiation shall be required to wear their personal TLD badge at all times inside the premises of the radiation oncology center. This shall be part of their uniform as an employee, and proper care of the TLD must be observed.Special restrictions apply to new and expectant mothers and it is essential that all such employees inform their RPO if they suspect that they are pregnant. A pregnant radiation worker will be reassigned to areas with lower radiation level, and such will be protected as a member of the public in the interest of protecting the embryo/fetus. The RPO will promptly review all monthly exposure reports from the PNRI to evaluate unexpectedly high or low exposures.
• The personnel dosimeters shall be worn either on the anterior chest area, lapels, or the waistline for effective estimation of the whole body dose.
• A permanent record of the results of each periodic dose evaluation of occupational exposure shell be kept on file for ready reference. The levels of investigation established for external exposures shall be used as the reference values for evaluating the radiation protection practices of each radiation workers (refer to Table 1).
• A rack will be set for proper monitoring and safekeeping of badges. The monitor must be placed at the rack provided by the radiation oncology center, and must not be brought home or elsewhere.
• Workers occupationally exposed to radiation should position the patients with the least possible effort and time. He/ she should minimize unnecessary conversation with patients and immediately proceed to implement the treatment protocol.
• Periodic quality assurance check of the therapy unit shall be done to ensure that all operational parameters of the units are within acceptable standards. The occupationally exposed worker shall be so controlled according to the recommendations of IAEA IBSS Safety Series 115.
a. effective dose of 20 mSv/year averaged over 5 years
b. effective dose of 50 mSv/year in any single year
c. equivalent dose to the lens of the eye of 150 mSv/year
d. equivalent dose to the extremities or skin of 500 mSv/year.
III. Local Rules and Supervision
A. Investigational Levels to Monitor Individual Occupational External Radiation Exposures
The Radiation Oncology Facility hereby establishes the Investigational Levels for individuals occupationally exposed to external radiation, such that when the values are exceeded, the RPO will initiate the necessary investigation and recommends appropriate actions.
Level I values are based on one-tenth (1/10) of the allowable 50 mSv, 500 mSv, and 150 mSv limit for one working year for the whole body, individual organs and tissues, and lens of the eyes doses respectively, averaged over a five (5) year period wherein a 20 mSv value shall not be exceeded (ICRP 50).
Level II values are based on a three-tenth (3/10) of the allowable 50 mSv, 500 mSv, and 150 mSv limit for only one working year period for the whole body, individual organs and tissues, and lens of the eyes doses respectively, averaged over a five (5) year period wherein a 20 mSv shall not be exceeded (ICRP 50).
Table 1. Investigational levels for protection for Ionizing Radiation
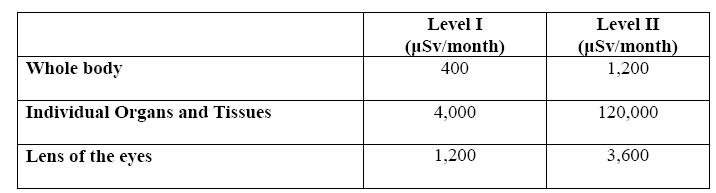
The RPO will review and record the results of personnel monitoring at least once in any calendar quarter. The values of effective doses shall be compared with the Investigational Levels in Table 1 and the following actions shall be taken.
1. Quarterly exposure of individuals less than Investigational Level 1.
Except when deemed appropriate by the RPO, no further action shall be take in those cases in which an individual’s exposure is less than the values in Table 1.
2. Quarterly personnel exposure greater than or equal to Level 1 but less than Level II.
The RPO will review the exposure of each individual whose quarterly exposure equals or exceeds Level I values and will report the results of such reviews to (1) the management and staff meetings following the quarter when the exposure was recorded. If the exposure does not equal or exceed Level II, no action related specifically to the exposure is required unless deemed
appropriate by the organization. The organization shall however consider each exposure in comparison with those others performing similar tasks as an index of ALARA quality program and shall make record of such during the review in the organizations minutes.
3. Quarterly personnel exposure equal to or greater than Level II
The RPO shall investigate in a timely manner the causes of all personnel exposures that are equal to if greater than Level II and if warranted, take appropriate action. A report of the result of the investigation, action taken if any shall be presented to the organization at the first meeting following the completion of the investigation. The details of these reports shall be recorded in the minutes of the meeting. Further, the minutes of the meeting shall be made available to PNRI and BHDT personnel for review or inspection.
B. Personnel Training Program
b1. Schedule of Training
Training will be provided:
• before an employee assumes duty with or in the immediate vicinity of the radiation source.
• annually as refresher training for all employees, and
• whenever a significant change occurs in duties, regulations of the terms of the radiation facility license.
b2. Description of Training
Training will be sufficient to ensure that:b3. Content of the Training Program
• individuals who work in or frequent controlled and supervised areas in the terms specified by the work duties of radiation workers.
• Individuals whose duties may require work in the immediate vicinity radiation sources are informed about radiation hazards and appropriate precautions.
The program of instruction will include:
• pertinent terms and conditions of the radiation facility license, including procedures developed as a prerequisite for obtaining a license and commitments incorporated into the license by condition.
• appropriate response to emergencies or unsafe conditions, including participation by appropriate dry runs of emergency procedures conducted as part of the initial and annual refresher training.
• areas where radiation is used
• potential hazards associated with radiation
• safety procedures appropriate to the duties of an employee
• pertinent BHDT and PNRI regulations
• obligations of all personnel to report unsafe conditions to the radiation protection officer
• the right of all personnel to be informed of radiation exposure
• location where the license has to be posted or made available. Copies of regulations and copies of radiation licenses and license conditions.
b4. Records that document the training
Records of initial and refresher trainings will be maintained until the BHDT terminates the X-ray license and will include:
• the name of the individual who conducted the training,
• the names of the individuals who received the training,
• the dates and duration of the training session, and
• the list of the topics covered.
C. Treatment Protocol
1. Clinical Evaluation and Therapeutic Decision
The onset of a radiation therapy treatment begins with the clinical evaluation of the radiation oncologist on the disease based on supporting histological, pathological and other examinations dose based on the patient’s condition. The radiation dose prescription shall come from the authorized user as defined in this ALARA Program duly registered with the BHDT and Philippine College of Radiology to treat patients of our facility. The radiation oncologist’s prescription shall be based on the Principles of Irradiation (please see below). No treatment shall be carried out unless radiation prescription is properly initialized by the authorized user on the patient’s chart. Further, treatment shall not commence without patient consent. Patients shall be asked to sign a waiver form prior to irradiation.
2. Imaging and Localization
The region of interest that needs to be treated shall be localized with the imaging tools available to locate the target volumes. The GTV, CTV and OAR (ICRU 50 and 62) shall be determined by the oncologist based on his clinical judgment, expertiseand experience. Other patient contour and organ segmentation maybe delegated to the physicist or radiation technologists for completeness. The radiation oncologist verifies all additional contour and segments prior to treatment planning and dosimetry.
3. Treatment Planning
Beam aperture design, field multiplicity and collimation shall be designed by both the radiation oncologist and physicist. It is the responsibility of the physicist to verify the beam data integrity and isodose distributions before a treatment plan is carried out. The best treatment plan is shall be decided upon by the radiation oncologist before execution keeping in mind ALARA exposures to organs at risk (OAR).
4. Port Verification
Plans are verified on the initial stage through the use of port films with the aid of
available modalities.
5. Treatment
On the first day of treatment, the radiation oncologist and his support staff establishes the set-up. Localization films, chart review and dosimetry checks are carried with the radiation therapy physicist and radiation therapy technologist. The use of immobilization devise and other accessories shall be further reestablished or checked. Indelible marks are drawn on patient skin to help aid in the reproducibility of set-up. On the course of treatment, proper patient identification shall be observed to ensure that the right patient and the right anatomy is irradiated. As part of patient identification, the patient is called with his /her name and random questions may be asked of him/her regarding his/her condition, treatment, picture, etc. This procedure also serves as a check on how well the patient understood the treatment process.

D. Principles on the Prescription of Irradiation
1. Evaluation of the full extent of the tumor (staging) by whatever means available, including radiographic, radioisotope and other studies.
2. Knowledge of the pathologic characteristics of the disease, including potential areas of spread that may influence the choice of therapy (e.g. rationale for elective irradiation of the lymphatics in the neck or pelvis).
3. Delineation of goal of therapy (cure versus palliation).
4. Selection of appropriate treatment modalities, which may be irradiation alone, or irradiation combined with surgery, chemotherapy, or both. The choice will have a significant impact on the volume treated and the doses of the irradiation delivered.
5. Determination of the optimal dose of irradiation and the volume to be treated, which are made according to the anatomic location, histologic type, stage, potential regional node involvement, and other characteristics of the tumor, and the normal structures present in the region. The radiation oncologist should never hesitate to modify established policies in order to tailor the treatment plan to the needs of the patient.
6. Evaluation of the patient’s general condition, periodic assessment of tolerance to treatment, tumor response, and status of the normal tissues treated.
"While the patient is under our care we take full and exclusive responsibility, exactly as does the surgeon who takes care of a patient with cancer. This means that we examine the patient personally, review the microscopic material, perform examinations and take biopsy if necessary. On the basis of this thorough clinical investigation we consider the plan of treatment and suggest it to the referring physician and to the patient. We reserve for ourselves the right to an independent opinion regarding diagnosis and advisable therapy and if necessary the right disagreement with the referring physician. . . During the course of the treatment, we ourselves direct any additional medication that may be necessary. . . and are ready to be called in an emergency at any time." - The Active Role of the Radiation Oncologist (F. Busche, 1962).
E. Treatment Planning Considerations in Pregnant Patients
1. Ensure that the dose to the fetus is kept to a minimum.
2. Complete all planning as though the patient were not pregnant.
3. Consider modifications of the plan that would minimize the fetal dose (changing field size and angle, etc.).
4. Estimate dose fetus without shielding using a phantom.
5. Design and construct special shielding if necessary.
6. Measure dose to the fetus in a phantom during simulated treatment with shielding in place.
7. Document the treatment plan and discuss it to all personnel involved with the treatment.
8. Monitor fetal size and location throughout the course of the therapy and update estimates of fetal dose if necessary.
9. Document the completion of treatment by estimating the total dose to the fetus due to the radiation therapy.
F. Management of Radiation Therapy Patients with Cardiac Pacemakers
1. Have the patient’s coronary and pacemaker status evaluated by a cardiologist before and soon after the completion of the therapy.
2. Always keep the pacemaker outside the machine-collimated radiation beam: both, during treatment and taking portal films.
3. Carefully observe the patient during the first therapy session to verify that no
transient malfunctions are occurring and during subsequent treatments if
magnetron misfiring (sparking) occurs.
4. Before the treatment, estimate and record the dose (from scatter) to be
received by the pacemaker. The total accumulated dose should not exceed
approximately 2 Gy.
5. If treatment within these guidelines is not possible, the physician should
consider having the pacemaker either temporarily or permanently removed
before irradiation.
IV. Quality Assurance
A. Radiation Protection of Personnel and Patients
TLD badges are required for all personnel who work frequently in the vicinity of the radiation therapy accelerator. This includes physicians, physicist, radiation therapists, accelerator maintenance personnel, and aides. Periodic radiation protection checks shall be carried out on both the machine and the facility. Checks on the facility include the door interlock
B. Security
Only authorized personnel can operate the linear accelerator. Authorized personnel include the medical physicist, radiation therapists and the authorized service engineer of the accelerator. The requisite security measures include requiring radiation therapists to carry the console key with them if necessary at times when the console is unattended and to lock up the console keys in a secure place after working hours.
C. Maintenance
The management, thru the medical physicist, is responsible for obtaining machine maintenance and for assuring that the accelerator is fit for use after maintenance, be it a repair or just preventive maintenance. For example, if repairs involved dosimetry components, the physicist shall check the machine output calibration (and perhaps flatness, symmetry, percent depth dose) before allowing the accelerator back to clinical service. A service log report shall be kept for this purpose.
D. Quality Control
Check source program
Place other programs here.
E. Structural Shielding
The radiation shields in the rooms adjacent to radiotherapy equipment are reasonably thick because the radiation emitted by high-energy treatment equipment is extremely penetrating and the dose rates used in radiotherapy are high. When the design of the radiation shielding was considered, the workload of the equipment and the way it is used, as well as the intended use of the areas adjacent to the treatment room and the occupancy of the areas in question for the new facility, was taken into account (Appendix 3?). The wall is further provided with a wall barrier (maze-type) of appropriate thickness in order to provide additional protection between the source of radiation and the main entrance door of the treatment room. Note: no modification was carried out on the main radiation barriers of the old facility for the year 2007.
F. Warning Signs, Alarm and Interlock Systems
A BEAM-ON and BEAM-OFF light signals are installed at the main entrance door to the treatment room to warn the public that radiation exposure is going on inside the treatment room. These warning signals are electrically coupled to an interlock relay switch that is mounted at the entrance door, which deactivates the BEAM-ON light signal when the door is open. The door interlock system automatically switch the x-ray source the off position whenever the door to the
treatment room is accidentally opened during the course of radiation treatment. A radiation warning sign according to international standards is conspicuously posted on the entrance door of the treatment room to keep unauthorized persons from entering the irradiation area.
G. Monitoring Instruments
Areas where work with ionizing radiation is undertaken must have immediately available suitable monitoring instruments. A survey meter will be routinely used to measure radiation at the level of the door and at the console room. The instrument must have an individual calibration prior to its initial use and the instrument must be examined and calibrated by a competent authority. A copy of the calibration certificate will be kept with the instrument. If such instruments are battery operated then a weekly check will be made on the condition of the batteries.
Calibration Program of Survey Meter
1. The survey instruments should be calibrated annually, before first use, and following repair. Any Secondary Standard Dosimetry Laboratory (PNRI or BHDT) can perform the calibration. See sample on Appendix 4.
2. If there is a check source, the constancy of the survey meter should be checked at regular intervals.
3. Records of Calibration should be retained for at least five years.
4. Batteries should be checked on a daily basis. Spare batteries should always be available.
5. The survey instrument should be stored in the control room at all times for easy access during treatment and in case of emergency.
V. System of Records
A. Personnel Exposure
Periodic results from the PNRI on personnel exposure shall be kept for reference for at least ten years before disposal. Unusual doses received by the individual shall be investigated and recommendations shall be done according to the investigational levels set by the radiation oncology center.
B. Area Survey
Place result here.
C. Instrument Tests and Calibration
1. Survey Meter
The survey meter shall be subjected to calibration for at least once a year at the Secondary Standard Dosimetry Laboratory PNRI or BHDT-DOH. Results of instrument calibration shall be kept for five years for monitoring and assessment of the performance, and wear and tear of the instrument.
2. Dosimetry Assembly (Electrometer, Ion Chamber and Extension Cable) The dosimetry assembly shall be subjected for calibration at least once a year at BHDT-DOH. Results of instrument calibration shall be kept for at least 10 years for monitoring and assessment of performance and wear and tear of the assembly.
D. Audits and Reviews of Radiation Safety Program
Results of audit and reviews shall be documented. All recommendations from the auditing team shall be noted and implemented in adherence to the ALARA principle.
E. Incident and accident investigation reports
An investigation shall be initiated by the Radiation Protection and Safety Officer of the facility and a report on the accident and incident involving ionizing radiation shall be issued. The report will include all machine parameters, irradiation time, accessories and treatment aides used. The cause of the incident shall be thoroughly investigated with the doses received by the involved parties accounted or approximated. Please see attached form.
F. Maintenance and repair work
All maintenance and repair work done by service and software engineers shall be noted the “service report” of the servicing party, and such will be confirmed both by the technician/engineer and the medical physicist. Documentation shall be kept on file and shall be consulted as necessary in the event that repairs and/or maintenance work need be carried out. Reasons for service and all actions taken will be noted down.
G. Facility Modifications
Alteration in any aspect of the facility that will affect radiation protection and safety of the workers, patients and the general public shall be logged by the medical physicist/radiation protection officer. The regulatory agency shall be properly notified if any modifications are carried out.
H. Training Provided
Refer to local rules and regulation.
I. Clinical Dosimetry Records
Documentation on dosimetry shall be filed together with associated tests/studies requested by the oncologist for clinical evaluation. The dosimetric calculation shall reflect the parameters and factors assumed including gantry, collimator and couch orientations, field sizes, weighting factors, inhomogeneity factors, attenuation, transmission and scatter factors and treatment time. It shall also include dose point data on the maximum dose or ICRU points if necessary (refer to ICRU Reports 50 and 62).
VI. Radiation Accident/Incident Report
The Radiation Oncology Facility defines a reportable radiation accident as:
a. actual or potential exposure of a worker to more than 5 mSv
b. actual or potential exposure of a member of the public to more than 1 mSv
c. the administration of external beam therapy or brachytherapy where the dose received differs by more than 15% from the prescribed dose.
The RPO with the help of the attending physician will furnish a report immediately after investigation to the BHDT concerning patients accidentally exposed. Information on the individual’s name, age, sex, occupation and classification will be furnished with the report as well as the detailed description of the accident/ incident. For therapeutic treatment delivered to the wrong patient, wrong tissue (site) or with dose fractionation substantially different from the values prescribed by the radiation oncologist, the report shall come with details of calculated or estimated dose received by the irradiated region. The distance between the patient and the source, the orientation of the patient to the source, and the part of the body which was exposed, the duration of the exposure, the presence of any shielding material between the source and the patient shall be considered.
Only patients are allowed to stay inside the treatment room during “BEAM ON.” Other individuals other than the patient who are accidentally exposed to ionizing radiation inside the treatment room during therapy shall be likewise investigated, as well as the dose they received will be calculated and estimated by the RPO. If the individual is a radiation worker, temporary suspension from work connected radiation hazards may be recommended as deemed necessary. No worker undergoing intervention shall be exposed in excess of the maximum single year dose limit for occupational exposure except:
a. for the purpose of saving life or preventing serious injury;
b. if undertaking actions intended to avert a large collective dose; or
c. if undertaking actions to prevent the development of catastrophic conditions (IBSS Safety Report Series 115).
After the accident, comprehensive records shall be maintained of assessments and their updates and of monitoring results for patients, workers, the public and the environment. The Radiation Accident/Incident Report contains:
• Name and address of facility
• Name of radiation protection and safety officer
• Brand/Model/Serial No. teletherapy equipment equipment/beam energy
• Vital information of the persons accidentally exposed such as name, age, sex,occupation and classification whether patient, worker or member of the general public
• Identification and detailed description of the accident/incident
• Cause of the incident/accident
• Dose calculation or estimation
• Corrective measures required to prevent recurrence of such accident/incident
• Corrective measures implemented
• Interventions taaken by the institution on the accidentally exposed persons. See sample form on Appendix 6
VII. Emergency preparedness&Response Plan
A. Safety Control System Failure
a1. X-ray beam fails to terminate when the accumulated dose displayed on the upper primary dose monitor (ACTUAL MON 1) exceeds the preset dose (SET MON 1). Follow the procedures below should this happen:
1. Press the INTERRUPT push button on the console. But if the beam remains ON,
2. Press the EMERGENCY OFF button in the console room, near the door or in the treatment room behind the gantry. But if the beam remains ON,
3. Switch off the "LINAC” breaker or the "MAINS" breaker in the power distribution box.
4. Remove the patient from the treatment room.
5. Report the incident immediately to RPO/physicist. Do not attempt to operate the linear accelerator until service personnel has verified proper operation, including emergency off circuits.
a2. Power Failure
1. If a patient were receiving therapy at the time of the power failure, record thea3. In case of Earthquake, Fire, Smoke or Gas Fumes
cumulative number of monitor units received up to the interruption. This value
is shown on the LCD back-up dosimetry display of the Treatment Control
Cabinet.
2. When the power is restored, do not attempt to operate the linear accelerator
until completing the daily start-up procedures.
1. Interrupt the treatment and transport the patient to a safe distance outside thea4. EMERGENCY OFF circuit fails to terminate
center.
2. Turn off the machine and lock the treatment room.
3. After the incident, cordon the area to prevent access of the public.
4. Notify the RPO, physicist, BHDT and/or the service engineer immediately
about the incident. Do not attempt to operate the linear accelerator until
completing the daily start-up procedures.
The EMERGENCY OFF circuit has failed to terminate if an EMERGENCY OFF button is pressed and the sound of the running motors within the treatment room continues or the power indicator on the console remains on.
1. Immediately turn off the main circuit breaker.B. Medical Exposure
2. If a patient were receiving therapy at the time of the EMERGENCY OFF failure, record the cumulative number of monitor units received up to the interruption. This value is shown on the LCD back-up dosimetry display of the Treatment Control Cabinet.
3. Do not attempt to operate the linear accelerator until service personnel has verified proper operation, including emergency off circuits.
Our facility is committed to adhere to the principles of Radiation Protection and IBSS Safety Reports Series 115 which includes among others:
b1. Responsibilities for Medical Exposure
a. Patient treatment or diagnosis using sources of radiation will be prescribed only by oncologists registered to treat patients in the facility.Justification
b. Calibration, dosimetry and quality assurance requirements for radiation diagnosis and therapy are conducted by or under the supervision of the medical physicist.
c. Authorized users must make arrangements to ensure an adequate number of trained personnel to discharge assigned tasks.
In line with this principle, our facility shall not allow any patient exposure either for diagnostic or therapeutic purposes unless such exposures are warranted to be medically beneficial by a
qualified physician. No patient will be administered a diagnostic or therapeutic medical exposure unless the exposure is prescribed by an authorized user defined by this document. The calibration, dosimetry and quality assurance requirements will be conducted by or under the supervision of by the medical physicist. We strongly discourage any practice requiring patient exposure for the sole purpose of conducting research with no medical benefit to the exposed individual/s arising from such radiological practice “No radiological practice shall be done unless its introduction produces a positive net benefit.”
Optimization
b2. Device for medical exposures:
a. Radiation producing devices will conform to applicable standards of the Bureau of Health Devices and Technology – Department of Health, the International Electrotechnical Commission (IEC) and the International Organization for Standardization or to equivalent standards as appropriate;b3. Calibration
b. Performance specifications and operating and maintenance instructions, including protection and safety instructions, will be provided to the users of radiation producing equipment;
c. Where practicable, the operating terminology (or its abbreviations) and operating values will be displayed on operating consoles. The facility shall implement prepare and adopt simple and easy to follow protocols well understood by personnel concerned with the abovementioned treatment processes so that the incidence of human error in the delivery of unplanned medical exposure is minimized. “All exposures shall be kept as low as reasonably achievable, taking into account social and economic factors.”
a. Radiotherapy equipment calibration will be determined and recorded in terms of radiation quality or energy and either absorbed dose or at a predefined distance under specified conditions. Factors shall be based to IAEA Technical Reports Series 398 recommendations, and literatures supported by the scientific community on dosimetry and metrology.b4. Investigation of Accidental Medical Exposure
b. Calibration will be carried out at commissioning of a unit, after maintenance that could affect dosimetry and at periodic intervals specified by regulation or by the Radiation Safety Committee.
The Radiation Health Safety Officer will be notified of and will promptlyb5. The accidental medical exposure report contains:
investigate any of the following incidents:
- Any therapeutic treatment delivered to either the wrong patient or the wrong tissue, or with a dose fractionation differing substantially from the values prescribed by the medical practitioner or which may lead to undue acute secondary effects;
- Any equipment failure, accident, error, mishap or other unusual occurrence with the potential for causing a patient exposure significantly different from that intended.
The RPO together with the user will calculate or estimate the doses received and their distribution within the patient. They will indicate the corrective measures required to prevent recurrence of such an incident.
- The user, with the RPO, will implement all the corrective measures that are under their own responsibility.
• Calculated/estimated doses received and their distribution within the patient.
• The corrective measures required to prevent the occurrence of such incidents/accidents.
• The implementation of all the corrective measures done and the person/s responsible to these corrective measures.
• Submission of a written report to the BHDT which states the cause(s) of the incident including all other information applicable.
• Information given to the patient and the doctor about the incident.
• Information concerning the medical aspects (if needed) in handling the externally irradiated person in the radiological accident.
References
1. CPR PART 3 - Standards for Protection Against Radiation. Philippine Nuclear
Research Institute.
2. ...and so many more, my apologies! I forgot most of them.
*****************************************************************************
Thanks Ms. Frances Caroline Lopez&Mr. Norberto Abella for your inputs!




Comments