But after SARS in 2003 and MERS a decade later, coronavirus has taken the world stage and it is never leaving the lexicon again. Every detected mutation is splashed across media outlets with no end in sight. Nearly everyone has to have been exposed at this point but well over 99 percent are unaffected and that leads to questions about how much more vaccines can help. Are antibodies from infection as good as a vaccination?
They can be, in a counter-intuitive way.
Some terms are in order; there is no such thing as "natural immunity" versus a synthetic kind - the vaccine creates a 'natural' response, that is the definition of a vaccine, so any immunity is natural. The only issue is which will be better. To get answers, a team looked at data from people who have been infected by SARS-CoV-2 but were not hospitalized as a result of the infection.
32 non-hospitalized COVID-19 positive Canadian adults were recruited by the Centre hospitalier de l’Université Laval 14 to 21 days after being diagnosed through PCR testing.
The results: Those who received the Pfizer BioNTech or AstraZeneca vaccine had antibody levels that were significantly higher than infected individuals. These antibodies were also effective against the Delta variant, which wasn't present when the samples were collected in 2020.
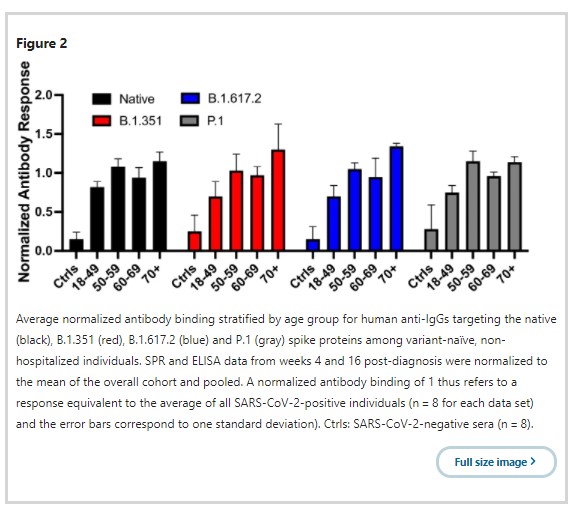
And older people with infections but didn't end up in the hospital produced more antibodies than younger people.
"Everyone who had been infected produced antibodies, but older people produced more than adults under 50 years of age," said Professor Jean-François Masson of Université de Montréal's Department of Chemistry. "In addition, antibodies were still present in their bloodstream 16 weeks after their diagnosis."
Antibodies produced after an infection by the original, "native" strain of the virus also reacted to SARS-CoV-2 variants that emerged in subsequent waves, namely Beta (South Africa), Delta (India) and Gamma (Brazil), but to a lesser extent: a reduction of 30 to 50 percent.
"But the result that surprised us the most was that antibodies produced by naturally infected individuals 50 and older provided a greater degree of protection than adults below 50, " said co-author Professor Joelle Pelletier. “This was determined by measuring the antibodies' capacity to inhibit the interaction of the Delta variant's spike protein with the ACE-2 receptor in human cells, which is how we become infected. We didn't observe the same phenomenon with the other variants."
The study is small, pilot results, but speak to the benefit of a vaccine even if someone was already infected and basically only had a bad cold. When someone who has had a mild case of COVID is vaccinated, the antibody level in their blood doubles compared to an unvaccinated person who has been infected by the virus. Their antibodies are also better able to prevent spike-ACE-2 interaction.
"But what's even more interesting," said Masson, "is that we have samples from an individual younger than 49 whose infection didn't produce antibodies inhibiting spike-ACE-2 interaction, unlike vaccination. This suggests that vaccination increases protection against the Delta variant among people previously infected by the native strain."





Comments