Up to 15 percent of Americans take an antidepressant while hydrocodone and codeine are often prescribed to patients who have recently undergone surgery. If they are taking an antidepressant and it leads to greater pain, they may want to increase their dosage. Because pain medication is prevalent they focused on surgical patients.
The researchers focused on the interaction between opioids and SSRIs because they knew that certain opioids, called prodrug opioids, need a liver enzyme to convert them into an active form that eases pain. SSRIs inhibit this enzyme, so the researchers hypothesized that patients taking SSRIs in combination with prodrug opioids would receive less pain relief. Prodrug opioids include codeine and hydrocodone, which is sold under brand names such as Vicodin, Lorcet and Lortab. SSRIs include Prozac, Paxil, Zoloft and Celexa.
For the study, the research team analyzed de-identified data for 4,306 surgical patients with a diagnosis or symptoms of depression in the electronic health records at Stanford Health Care.
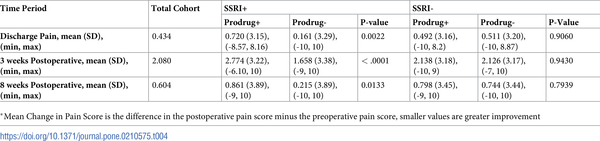
The researchers found that the patients on SSRIs who were prescribed prodrug opioids experienced more pain when they left the hospital, as well as three weeks later and eight weeks later. The patients on both SSRIs and prodrug opioids registered nearly one point more pain on a scale of 1 to 10 than the patients not on SSRIs who were prescribed prodrug opioids.
The researchers built a machine-learning algorithm that predicts how a patient will respond to different types of opioids.





Comments