Researchers have successfully modeled using both familial and sporadic patient-derived induced pluripotent stem cells (iPSCs), and revealed stress phenotypes and differential drug responsiveness associated with intracellular amyloid beta oligomers in
Alzheimer's disease
neurons and astrocytes.
The researchers generated cortical neurons and astrocytes from iPSCs derived from two familial AD patients with mutations in amyloid precursor protein (APP), and two sporadic
Alzheimer's disease
patients. The neural cells from one of the familial and one of the sporadic patients showed endoplasmic reticulum (ER)-stress and oxidative-stress phenotypes associated with intracellular amyloid beta oligomers.
The team also found that these stress phenotypes were attenuated with docosahexaenoic acid (DHA) treatment. These findings may help explain the variable clinical results obtained using DHA treatment, and suggest that DHA may be effective only for a subset of patients.
Using both familial and sporadic
Alzheimer's disease
iPSCs, the researchers discovered that pathogenesis differed between individual AD patients. For example, secreted amyloid beta 42 levels were depressed in familial AD with APP E693 delta mutation, elevated in familial
Alzheimer's disease
with APP V717L mutation, but normal in sporadic AD.
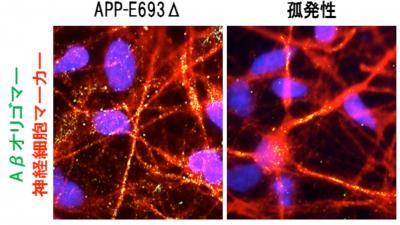
This shows amyloid beta oligomers in neurons from a familial AD (APP-E693 delta) (left) and from a sporadic AD patient (right). Credit: Courtesy of Dr. Haruhisa Inoue laboratory
"This shows that patient classification by iPSC technology may contribute to a preemptive therapeutic approach toward AD,'' said Associate Professor Haruhisa Inoue of the Center for iPS Cell Research and Application (CiRA) at Japan's Kyoto University . "Further advances in iPSC technology will be required before large-scale analysis of AD patient-specific iPSCs is possible.''
Published in Cell Stem Cell






Comments