That requires modern tools like CRISPR-Cas9 and others. Tools that environmentalists oppose, insisting all science is a corporate conspiracy. As they have historically done with natural gas and GMOs and vaccines. Antiretroviral therapy is highly effective at suppressing HIV, so the virus is no longer the direct death sentence it once was, but the immune system remains in an inflammatory state of overactivation and impaired functionality.
That places those with the virus at greater risk of co-morbidities, like tuberculosis. Which can be prevented if scientists are allowed to approve advanced treatments without worrying that the activist community will destroy their careers, or lobby government to oppose breakthroughs, as has historically been their tactic.
New work worked on latent TB, iwhen Mycobacterium tuberculosis (Mtb) is present but not causing active symptoms of disease and is not infectious, and its impact on those with HIV.
About 2 billion people globally have latent TB. In the U.S. alone, 13 million people are estimated to have the bacteria. The vast majority do not fall ill, but those with HIV have a higher risk for developing active TB, making it the leading cause of death for those with co-infection.
The current protocol for HIV is antiretroviral therapy plus the antibacterial protocol 3HP to minimize chances of activating latent tuberculosis, but the new study found that the issue remains because the immune system does not reset to a more normal state. The work with SIV, the primate version of HIV, revealed that specific populations of T cells - white blood cells that are a key component of the immune system - were imbalanced following treatment compared with the control group. There were fewer CD4+ effector memory T cells, which send early signals to other immune cells to attack. A subset of beneficial T helper cells (TH1) were decreased, while another T cell type (TH17) was increased and may be responsible for continuous immune system activation.
Using single cell RNA sequencing, the team also tracked the activity of macrophages – which are large immune cells that engulf Mtb in the lungs – at the beginning of infection. Macrophage functionality, determined through which genes were turned on or off, changed as early as two weeks after co-infection with SIV and did not change back after completing the treatment regimens.
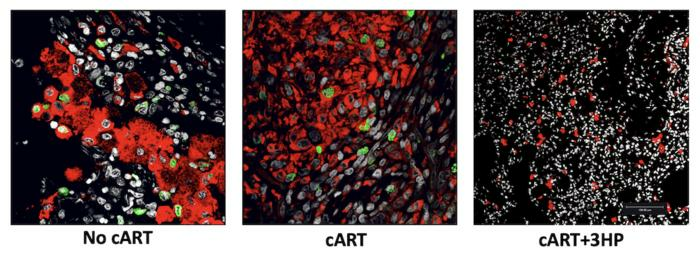
Red macrophages and green proliferating macrophages in lung tissue. Macrophage turnover is significantly reduced in the lungs of cART+3HP-treated macaques (right) compared to animals treated with cART alone (middle) or untreated controls (left). While reduced turnover indicates decreased cellular replacement, additional functional changes observed in these macrophages suggest that the population remains dysregulated and retains inflammatory characteristics during chronic infection, despite treatment. Credit: Texas Biomed
Treating a virus but not helping the immune system is not just a risk for HIV, everyone with respiratory diseases would benefit, but that requires advanced tools. The kind of thing activists oppose. With people on the left now abandoning issues they once ignored because it was their political party, perhaps the newfound embrace of science will mean pushing back in areas like food, energy, and medicine. Then scientists will be allowed to make real progress in issues like this, and not consider it a waste of time because lawyers will use regulations they created to block progress against people who want to lead us into the future.
Citation: Sharan, R., Zou, Y., Singh, B. et al. Concurrent TB and HIV therapies control TB reactivation during co-infection but not chronic immune activation. Nat Commun (2025). https://www.nature.com/articles/s41467-025-67188-4






Comments