Erin wrote an excellent article last year on SAD, and I don't want to repeat what she's already written. A few updates have been published in medical literature, however, so it's worth reviewing and bringing SAD sufferers up to speed.
What is Seasonal Affective Disorder?
SAD is "a subtype of recurrent depression that characterizes an estimated 10% to 20% of all cases of recurrent depression" and in clinical diagnosis is a "modifier to be applied to recurrent forms of mood disorders, rather than as an independent entity."1, 2 As leaves change color with the seasons, so does the color of our mood turn from a sunny spring and summer yellow to a wintery blue and gray.
 SAD sufferers enter a vegetative-like state, in which they are tired, depressed, anxious, and withdrawn. More women are affected by SAD (about 3:1), and there is an association between SAD prevalence and distance from the equator (farther away from the equator = more cases of SAD). While 18 million Americans have SAD, another 15% (or 45 million) experience a few mild SAD symptoms during the fall and winter seasons. By spring, most experience complete remission.3
SAD sufferers enter a vegetative-like state, in which they are tired, depressed, anxious, and withdrawn. More women are affected by SAD (about 3:1), and there is an association between SAD prevalence and distance from the equator (farther away from the equator = more cases of SAD). While 18 million Americans have SAD, another 15% (or 45 million) experience a few mild SAD symptoms during the fall and winter seasons. By spring, most experience complete remission.3The criteria for a SAD diagnosis have changed over the years, and it can now be a co-morbidity (i.e. bipolar and SAD), whereas early on it was only a subtype of major depressive disorder and could not be diagnosed in conjunction with any other mood disorder.
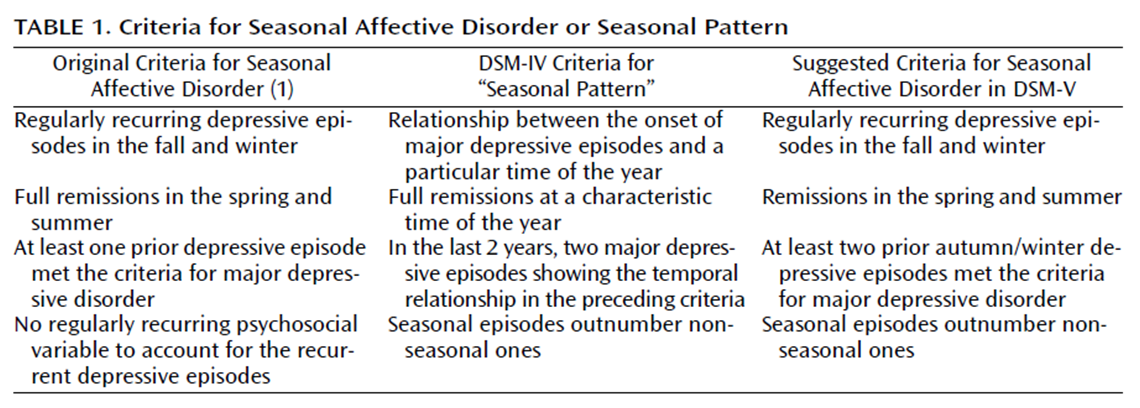
Rosenthal2 suggests that DSM-V be updated to "recognize the scientific basis for the validity of this disorder as an entity and provide it with a category of its own."
What causes SAD?
There are multiple theories as to the cause of SAD, but so far there isn't a conclusive answer. The front runner is light sensitivity - sunlight affects the body's regulation of sleep, hormones,
 and mood, so less exposure to sunlight in the fall and winter could affect these and contribute to SAD symptoms.
and mood, so less exposure to sunlight in the fall and winter could affect these and contribute to SAD symptoms.Other possible underlying causes include neurotransmitter deficiencies, low levels of Vitamin D, impaired ocular processing of light, or seasonal changes in melatonin secretion. Most likely, though, the cause of SAD is multifactorial. The Wall Street Journal notes several odd findings that seem to contradict a single explanation.
Why do SAD symptoms tend to peak in January and February, even though days are lengthening by then? Why does it hit most prominently between the ages of 18 and 30, and why are women three times as likely as men to be affected? The incidence of SAD is also surprisingly low in Iceland, where the homogenous population leads experts to surmise that genetic factors may also play a role.SAD symptoms can be alleviated by pharmaceuticals, vitamin supplements, exercise, psychotherapy or diet. Most often, however, physicians use light therapy to treat SAD symptoms. Generally patients are exposed to light daily for about three to six months until symptoms subside. However, it doesn't work for everyone (it's effective about 50 percent of the time), and not everyone sticks with it - it is estimated that only 41 percent continue regular use of light therapy. And the kicker - it doesn't prevent SAD recurrence the following year.
Treating SAD symptoms - two pilot studies
Background: The central public health challenge in the overall management of SAD is
prevention of the recurrence of depressive episodes over subsequent winter seasons, according to Rohan et al.3 Light therapy is the most effective current treatment, but as I said above it's a burden on time (daily for 3-6 months) and patients don't always stick with it. The researchers wondered if they supplemented light therapy with an acute (time-limited) therapy, would that improve symptoms, and could it possibly help prevent recurrence? So, they devised two small pilot studies (n=69) to compare standard light therapy alone with SAD-tailored group Cognitive Behavioral Therapy alone4 or both. They hypothesized that initial treatment with CBT or with CBT combined with light therapy would be associated with a smaller proportion of recurrences of depression (1 year after treatment completion), less severe symptoms, and a higher proportion of remissions in the next winter than initial treatment with light therapy.
Methods: Participants met DSM-IV criteria for Major Depression, Recurrent, with Seasonal Pattern on the Structured Clinical Interview for DSM-IV Axis I Disorders—Clinician Version with no comorbid Axis I disorder and met the threshold for a current SAD episode as assessed by the Structured Interview Guide for the Hamilton Rating Scale for Depression—Seasonal Affective Disorder Version.
Participants in the feasibility pilot study were randomly assigned to one of three 6-week conditions: group CBT, light therapy (LT), or a combination. Participants in the controlled, randomized pilot study were randomly assigned to one of four 6-week conditions: one of the same three active treatment conditions as in the feasibility study (i.e., CBT, LT, and CBT + LT) or a concurrent wait-list control (i.e., a minimal contact/delayed light therapy control).
CBT was conducted in small group format for 1.5-hour sessions twice a week over the 6 weeks (total of 12 sessions) following the tailored manual; LT was initiated using a 10,000-lux SunRay light box in two 45-minute daily doses in the morning and evening. In the controlled, randomized trial, after 1 week, an expert light therapy consultant individually tailored the time of day for light administration to maximize response, address evident phase shifts, and reduce side effects. After 6 weeks of supervised LT, participants could elect to continue using LT through the end of April and were asked to return the light box in May. Participants who were randomized to CBT, LT, or CBT + LT and who had not dropped out of the study by the end of acute treatment phase were invited to return to the laboratory for a naturalistic follow-up visit during the subsequent winter season.
The most important and meaningful outcome in a long-term follow-up of SAD is whether or not there was a recurrence in the next year as opposed to time to recurrence or episode duration.
Results: So, how did the various treatment groups fare? The proportion of depression recurrences at 1 year in participants randomized to CBT or to CBT + LT was significantly smaller than in participants randomized to LT alone (p = .020, p = .008 respectively). There were no statistically significant differences between combined CBT + LT and LT alone on any other outcome. CBT alone was also associated with significantly less severe depression at one year on the SIGH-SAD, (p = .019), the HAM-D component scale of the SIGH-SAD, (p = .006), and the BDI-II (p < .001) than LT alone.
Regarding full remission status at 1-year, CBT alone had a significantly larger proportion of
BDI-II-defined remissions at 1 year than the LT alone and CBT + LT groups (p = .001, p = .044, respectively). The treatment groups did not significantly differ on the SIGH-SAD remission outcome; but, descriptively, the trend in the data suggested an advantage of CBT alone (58.3%) over LT alone (30.1%). When the researchers looked at whether participants were in ongoing treatment, the only significant difference was a larger proportion of ongoing treatment in the LT group than in the CBT + LT group.
Conclusions: Initial treatment with CBT, with or without adjunct LT, was associated with a significantly smaller proportion of recurrences of depression relative to initial treatment with LT during the subsequent winter in the ITT sample. Initial treatment with solo CBT may lead to a more parsimonious course of action the next winter and, therefore, may be the best course off action given that SAD is a regularly recurring subtype of depression and that a long-term focus on prevention is arguably more important than a short-term focus on achieving an optimal acute treatment response.
I can see the light
Besides light therapy and the above mentioned treatments (e.g. antidepressants, exercise, etc) there are two new age sounding therapies SAD sufferers can try: negative air ions or dawn simulation.
Negative air ions are oxygen molecules naturally charged with extra electrons - WSJ gives the examples of air near a pounding surf or after a lightning storm. "One theory is that inhaling so-called superoxygenated air raises the oxygen level of the bloodstream as it pumps to needy tissues in the body."
Dawn simulation is just what it sounds like - you simulate dawn in your bedroom. A device "gradually turns the light on in your bedroom, creating a slow transition from darkness to dawn in the room while it's still dark outside. Even though the user is still asleep, and the maximum light is much dimmer than traditional light therapy, a few studies have found that dawn simulation can ease depression and help people wake up with more energy."
1 Behavior Therapy. Sept 2009. Vol 40(3), 225-238
2 Am J Psychiatry. Aug 2009. 166(8), 852-853
3 There are people who are actually the reverse, and exhibit SAD symptoms in the summer. Thus, says Rosenthal, it would be useful to provide the modifiers "with winter worsening" and "with summer" when making a diagnosis.
4 The SAD-tailored CBT treatment "is based on Young's dual vulnerability model for SAD involving a biological and a psychological component. The treatment is designed to target maladaptive cognitions and behaviors that have been shown to correlate with SAD (i.e., a possible psychological vulnerability), including dysfunctional attitudes, a negative attributional style, negative automatic thoughts, rumination, and behavioral disengagement."





Comments