(NEW YORK, NY)--Low levels of serotonin in the brain are known to play a role in depression and anxiety, and it is customary to treat these disorders with medications that increase the amount of this neurotransmitter. However, a new study carried out by researchers at Columbia University Medical Center (CUMC) suggests that this approach may be too simple. It appears that neighboring serotonin-producing brainstem regions exert different and sometimes opposing effects on behavior.
The findings, published today in the online edition of Cell Reports, provide new insights into the development of mood disorders and may aid in designing improved therapies.
"Our study breaks with the simplistic view that 'more is good and less is bad,' when it comes to serotonin for mood regulation," said study leader Mark S. Ansorge, Ph.D., assistant professor of psychiatry at CUMC and research scientist at New York State Psychiatric Institute. "Rather, it tells us that a more nuanced view is necessary."
Psychiatry
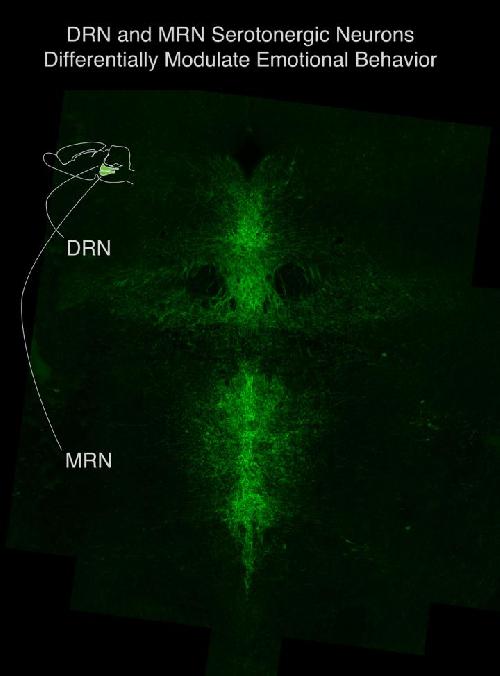
From anatomical studies, researchers knew that the brainstem contains two distinct clusters of serotonergic neurons: one in dorsal raphe nucleus (DRN) and another in the median raphe nucleus (MRN). Together both regions harbor the vast majority of neurons that supply serotonin to the rest of the brain, but it was unclear how neuronal activity within these clusters controls behavior.
To learn more, the CUMC team used a technique called pharmacogenetics to control the activity of serotonergic neurons in the DRN and MRN in both normal mice and in a mouse model of depression- and anxiety-like behavior. (The model was created by giving mice the drug fluoxetine shortly after birth, which produces long-lasting behavioral changes.)
The experiments revealed that alterations in serotonergic neuronal activity in the DRN and MRN produce markedly different behavioral consequences.
"Going into the study, our hypothesis was that reduced activity of serotonergic neurons is what drives these mood behaviors," said Dr. Ansorge. "But what we found was more complicated. First, it appears that hyperactivity of the MRN drives anxiety-like behavior. We also observed that decreased DRN activity increases depression-like behavior, while decreased MRN activity reduces it. This led us to conclude that an imbalance between DRN and MRN activity is what leads to depression-like behavior."
"This new understanding of the raphe nuclei should help us better understand why certain medications are effective in treating depression and anxiety, and aid in designing new drugs," Dr. Ansorge added. "In the future, it may be possible to find treatments that selectively target the DRN or the MRN, or that correct any imbalance between the two."
Jeffrey Lieberman, M.D., chair of the department of psychiatry at CUMC, observed that "Neurobiological studies such as this are essential to elucidate the molecular mechanisms of antidepressant treatments and to develop more effective therapies."
The study also demonstrated, in experiments using the fluoxetine-treated mice, that inhibition of serotonin reuptake early in life leads to long-lasting imbalances between the DRN and MRN. "This raises possible concerns about exposure to serotonin-specific reuptake inhibitors during gestation," said Dr. Ansorge. "SSRIs cross the blood-brain barrier as well as the placenta, and bind maternal and fetal serotonin transporters alike. It's too early to say whether this has any effect on behavior in humans, but it's certainly something worth looking into."






Comments