A new paper offers an explanation for the linear growth of the infection curve.
Traditional epidemiological models required so much fine-tuning of parameters that they became scientifically meaningless. Linear growth, with an R number at 1, in the epidemiology models that were being used would have to mean reducing contacts by the same exact and constant percentage. That was never going to happen outside the world of statistical hope.
The probability to observe linear growth in such standard compartmental models is practically zero, which means the real world needed something better.
There was cleary exponential growth early. An infected person would infect a few others, and in a chain reaction, those would pass the virus on to a few others as well. Social distancing was said to be the way to push the growth rate below the recovery rate and reduce the number of new infections. Individuals infect less than one other person, and the curve flattens, eventually reaching zero. Yet that did not happen either.Instead, there was a constant level of infections with a similar number of new infections every day, something academic epidemiological models find basically impossible.
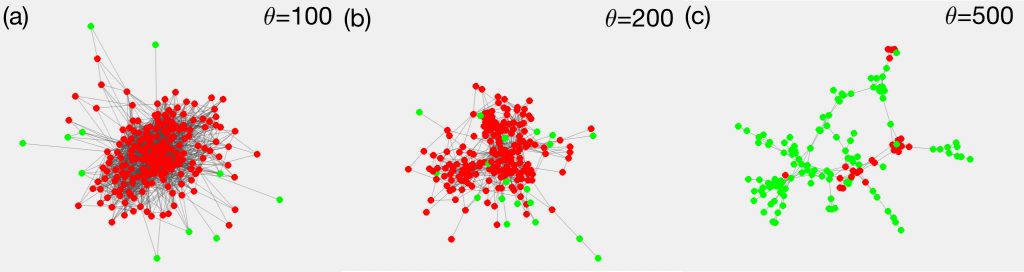
The figure shows a contact network of employees in an office building in France, thresholded according to the number of contacts.In (a) all links are shown that connect two persons with more than 100 encounters, (b) and (c) show the cases for 200 and 500 encounters. In the densest network (a) almost all employees get infected (red). Only a few with weak ties to the network’s core stay healthy (green). The same is true for the less dense network (b).Below a certain link density, things change abruptly (c): only a few infection clusters appear, while the majority remains healthy. This is the typical pattern observed in the COVID-19 pandemic when implementing social distancing measures. That shows the importance of reducing the network density below the critical point.
The linear shape of the curves is explained through a different form of spreading than initially expected: the spreading dynamic continued in small and limited clusters. Most people went to work, got infected and spread it to two or three people at home, and then those people went to work or school again. The infection was basically spreading from cluster to cluster.
It's a network effect, not a superspreading event, that made it linear
In the paper, the scientists showed that there is a critical number of contacts, which they call degree of contact networks or Dc, below which linear growth and low infection prevalence must occur. They found Dc to equal 7.2, assuming that people circulate in a coronavirus-relevant network of about five people, which is even lower during an effective lockdown (household-size 2.5 people on average).
Instead of having to fine-tune parameters, their model allows for a wide range of possibilities that keep the infection curves linear. It explains why linear infection curves appear in so many countries, irrespective of the magnitude of the imposed non-pharmaceutical interventions.
In a further step the scientists compared Austria, a country which responded with a severe lockdown early on, and the United States, which initially did not impose severe measures, and their model works for both scenarios: Both showed linear curves, but in the case of the US these just happened on a much higher level.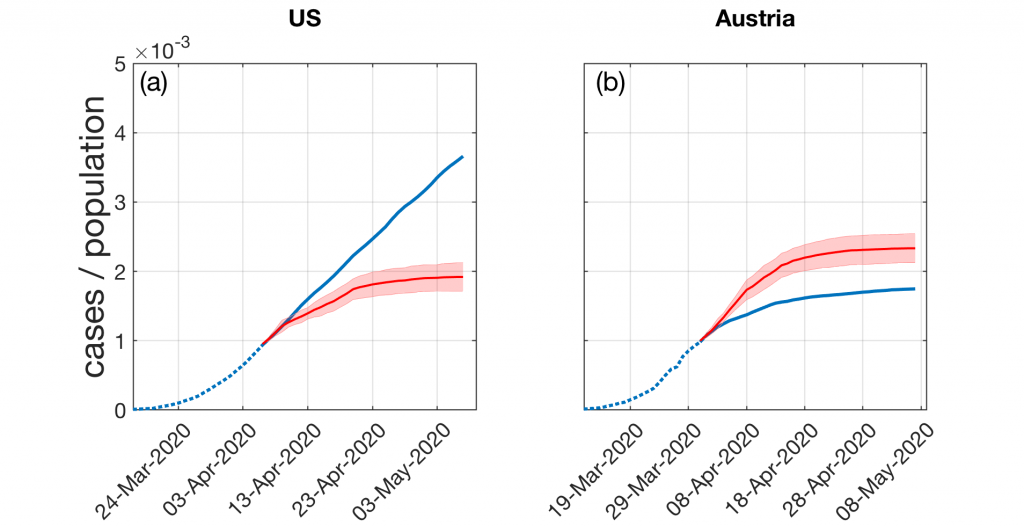
What if measures reduced the average degree in contact networks from five to 2.5 people early on? This could have almost halved the number of COVID-19 infections until the first week of May.What if Austria would have implemented its strict measures against coronavirus spread ten days later? According to the model, such a delay would have resulted in up to 30% more cases.
The model not only explains the emergence of a linear growth regime, but also explains why the epidemic could halt below the levels of herd immunity by consequent social distancing. For the standard modeling procedure, the complexity scientists use a so-called compartmental model with SIR-models, extending it with the described cluster transmission.





Comments