Researchers as St. Jude Children’s Research Hospital have alleviated sickle cell disease in mice using gene therapy methods. Their studies found that treated mice showed no distinction from normal mice. Even though it’s still too early to proclaim viable gene therapy for human diseases, this research is a vital piece of the puzzle.
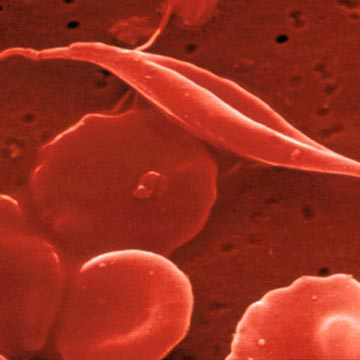
The image shows normal rounded blood cells and a "sickle" shaped blood cell affected by abnormal hemoglobin production. Photo credit: University of New Mexico
Their research showed treatment for long-term anemia and subsequent organ damage caused by the anemia. Sickle cell disease, a recessive condition affecting millions of people globally, is caused by a genetic defect in the gene coding for the hemoglobin component beta-globin. Hemoglobin is responsible for binding oxygen and carbon dioxide in blood cells. This defect causes abnormal hemoglobin function, causing deformation, clumping and breaking of the protein and blood cells. This can lead to clogged blood vessels, causing strokes and organ damage. The only treatment for sickle cell is a bone marrow transplant, allowing new blood cells to be cycled in the body. Such transplants are rare due to the lack donor compatibility and requirement of immunosuppression therapy for recipients.
Scientists studying sickle cell have known that the disease could be eliminated by introduction and maintenance of fetal hemoglobin, which contains gamma-globin, therefore avoiding the corruption of beta-globin. Researchers at St. Jude found that treating patients with hyroxyurea helps produce formation of fetal hemoglobin in adults and in turn, alleviate symptoms associated with sickle cell.
"While this is a very useful treatment for the disease, our studies indicated that it might be possible to cure the disorder if we could use gene transfer to permanently increase fetal hemoglobin levels," said Derek Persons, M.D., Ph.D., assistant member in the St. Jude Department of Hematology.
Persons and colleges developed a method for transferring the gene for gamma-globin into blood producing cells, using a viral agent. After re-introducing the blood forming cells into their mice, the researchers observed that they continued to produce gamma-globin, permanently generating normal red blood cells, which alleviated sickle cell disease. Their results, published in Molecular Therapy, saw that after months of the initial gene therapy, the mice continued to produce gamma-globin in their red blood cells.
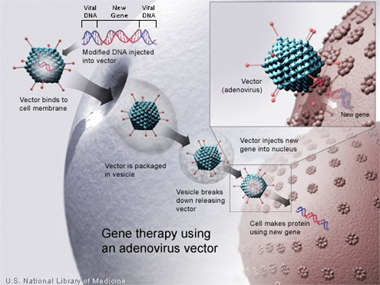
This image depicts gene therapy methods using an altered virus as a delivery system. The gene is placed into the virus, which inserts the gene into the cell, as it would for viral genes. The genes then take root in the cell and proliferate as part of the DNA sequence, correcting the genetic defect previously enacted in the cell. Photo Credit: Genetics Home Reference-National Institutes of Health
"When we examined the treated mice, we could detect little, if any, disease using our methods," said Persons. "The mice showed no anemia, and their organ function was essentially normal."
Further hopes for this method of gene therapy are supported by the permanence of the genes after the initial introduction. In a second set of tests, the researchers also transplanted the altered blood forming cells from the originally tested mice into a second generation of sickle cell mice. Five months after the transplant, the second generation mice also showed continued production of fetal hemoglobin and correction of their sickle cell.
"We are very encouraged by our results," Persons said. "They demonstrate for the first time that it is possible to correct sickle cell disease with genetic therapy to produce fetal hemoglobin. We think that increased fetal hemoglobin expression in patients will be well tolerated and the immune system would not reject the hemoglobin, in comparison to other approaches."
Persons’ laboratory is currently working with other animal models and human cells to develop better methods for gene insertion and production of fetal hemoglobin as a permanent and viable treatment for sickle cell disease.






Comments