The reason is that doctors may be unable to spend enough time with them.
It's not that doctors are unable or unwilling to do the job but time is limited and the Affordable Care Act and states have mandated that everyone must have insurance. In a state like California, everyone is required to carry health insurance but the regulatory and legal climate is so onerous there are nowhere near enough doctors to meet the mandated demand.
As a result, even though everyone has health insurance the first question most health care offices ask is what kind of health insurance patients have. If it is ACA, commonly called Obamacare, the wait may be substantial, if doctors accept them at all. That means there is a greater time crunch for doctors who will take any patients regardless of health insurance, and the trade-off may be a shorter visit.
'Pain' is a subjective description. Marijuana was made legal in many states because 'medical' marijuana prescription were overwhelmingly obtained by young men while middle-aged women actually repor a lot more pain. It was ridiculous to penalize women for being honest but young men got away with fake prescriptions because doctors need to practice defensive medicine when lawyers are waiting to sue, they may simply believe patients and prescribe painkillers. They may not want to be called out for "gaslighting" patients who claim they are in paid. The cultural damage if they don't take patient claims at face value is virtually unlimited.
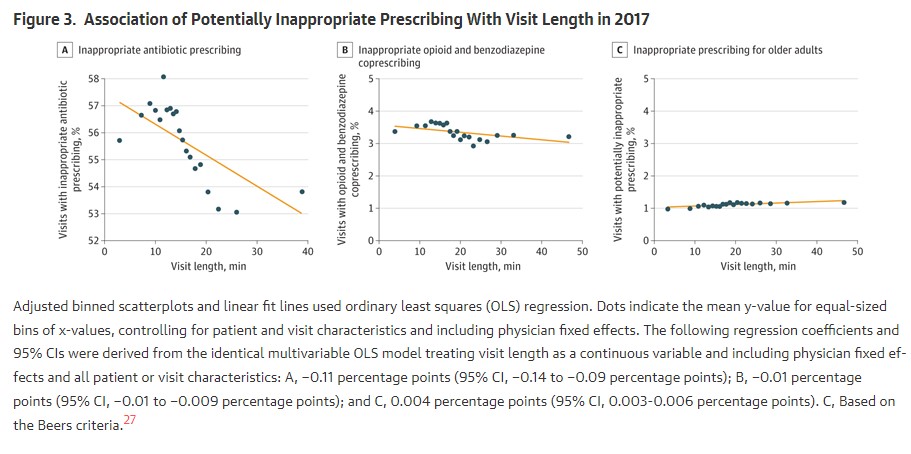
Shorter visits are not a knock on doctors. I want all of my doctor visits to be brief. There is no evidence that shorter visits mean worse care so this analysis looked at visit time and prescriptions. The results were that for each additional minute a doctor spent with a patient, the chance of inappropriate antibiotic prescription changed by −0.11 percentage points while likelihood of opioid and benzodiazepine coprescribing changed by −0.01 percentage point.
What does that mean? This is just exploratory so it means nothing but if people on subsidized insurance are having a harder time seeing doctors, we need more doctors. The solution is not to push out more osteopaths or, in the worse case, consider crackpots like naturopaths and homeopaths real doctors, but to ease the regulatory burden so that doctors can spend more time treating patients. California would be the fifth largest economy in the world if it were its own country, it has lovely weather, and yet doctors don't want to move here despite tremendous demand and high income.
The reason is regulations, and treating anyone with a business like they are a criminal waiting to happen. This correlation will be used as just that kind of weapon. Doctors are going to get sued if they deviated from an average and prescribed 'too much' based on short visits they need to have if they are going to see all of the patients needing to be seen.
That is a cultural problem created by government but patients are paying the price. However, one recommendation is solid and easy to implement, given that the federal government has forced a 'teach to the protocol' environment in medical schools and therefore medical practice; make upper respiratory tract infection visits longer as part of the protocol. That is automatically going to mean fewer antibiotics prescriptions, without lawsuits from lawyers waiting to force a settlement if doctors don't do what patients demand.





Comments