But it's actually the defensive medicine to not need to use malpractice insurance, along with medical culture that is told to teach to the protocol rather than think, that has caused health care costs to skyrocket. Defensive medicine is the practice of performing additional tests and procedures to have all of the proper boxes checked off in any possible deposition, even if a doctor knows they are a waste of time and money. In the early culture war on insurance companies, the refrain was 'my doctor should decide, not an HMO' but the modern climate is even worse. Lawyers are deciding by waiting in the wings and we are now all footing the bill for those hidden costs. Plus, with the new government-run health care system, not obeying a government protocol that defies medical judgment could mean a jail sentence.
A new analysis finds that 80 percent of U.S. neurosurgeons practice some form of defensive medicine. As you might expect, the rates and costs of defensive medicine are especially high in states with high-risk liability environments. "Although ordering extra laboratory tests, imaging studies, etc. was prevalent everywhere, it was even more so in high-risk states," according to the survey study by Dr. Timothy R. Smith of Northwestern University, Chicago, and colleagues.
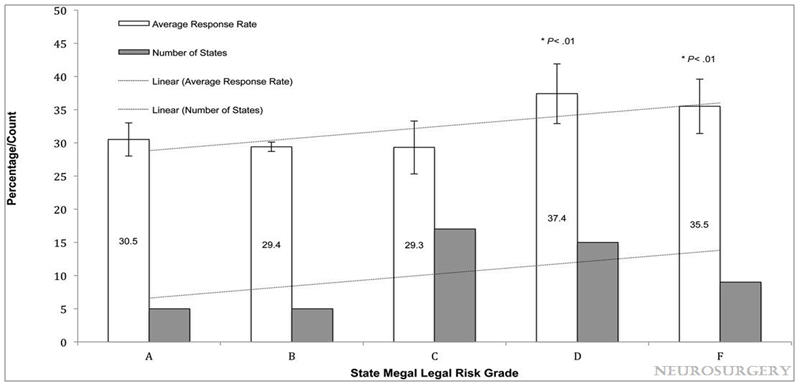
Relationship of state medicolegal risk grade to US neurosurgeon response rate. The National Report Card on the State of Emergency Medicine: A-F, grade A: Colorado, Texas, Kansas, Georgia, South Carolina; grade B: Idaho, Montana, Alaska, California, Oklahoma; grade C: Nevada, Arkansas, Nevada, North Dakota, Wisconsin, Hawaii, Louisiana, Ohio, Mississippi, West Virginia, South Dakota, Maryland, Utah, Virginia, Tennessee, Minnesota; grade D: Florida, Maine, Indiana, New Mexico, Alabama, Iowa, Massachusetts, Illinois, Connecticut, New Hampshire, Oregon, Pennsylvania, Maryland, Washington, Michigan, Wyoming; grade F: New York, Vermont, Delaware, North Carolina, Kentucky, Arizona, Rhode Island, New Jersey, District of Columbia, Oregon, Pennsylvania, Maryland, Washington. Credit: 10.1227/NEU.0000000000000576
The authors sent a questionnaire regarding defensive medicine to 3,344 Board-certified neurosurgeons. Defensive medicine refers to making medical decisions based on concerns over possible malpractice lawsuits, rather than any expected benefit to the patient. The study assessed the relationship between defensive medicine practice and an objective measure of the "liability risk environment" of the neurosurgeon's state.
The survey response rate was 31 percent, with 1,026 neurosurgeons responding. Most neurosurgeons correctly perceived their state's level of liability risk and those practicing in states with high-risk liability environments were more likely to respond.
Based on the survey responses, "The vast majority of US neurosurgeons participate in some form of defensive medicine," Dr. Smith and colleagues write. More than 80 percent of surgeons said they had ordered imaging tests solely for defensive reasons, while more than three-fourths reported ordering laboratory tests and making extra referrals for defensive purposes. Up to half said they ordered more medications and procedures out of fear of being sued.
Half of neurosurgeons are unwilling to do anything that might get them sued
Rates of all of these defensive behaviors included a 30 percent increase in the likelihood of ordering additional imaging studies for defensive purposes, 40 percent for additional laboratory tests and nearly half of neurosurgeons in high-risk states said they had stopped performing high-risk procedures because of liability concerns. Nearly one-fourth had stopped performing brain surgery for fear of being sued, while close to 40 percent were considering retirement because of the local liability environment.
Overall, the rate of defensive medicine behaviors increased by 50 percent at each grade of the five-point risk scale. Thus, a neurosurgeon practicing in a state at highest risk of liability would be six times more likely to practice defensive medicine than one in a state at lowest risk.
Neurosurgeons in high-risk states paid almost twice as much in malpractice insurance premiums as those in low-risk states. Across states, most neurosurgeons believed their malpractice coverage was inadequate. Malpractice premiums cost 15 to 20 percent of the neurosurgeons' annual income.
Neurosurgery--like obstetrics/gynecology and orthopedic surgery--is a specialty with a high risk of costly malpractice claims. Amid ongoing debate over defensive medicine, few studies have focused on the extent of defensive medicine practice among neurosurgeons.
The new survey suggests high rates of defensive medicine practice among neurosurgeons, and finds that these behaviors are related to perceived and actual liability risk by state. "Defensive medicine practices do not align with patient-centered care, and may contribute to increased inefficiency in an already taxed health care system," Dr. Smith and coauthors conclude.
It's hard to blame them. We have created a culture where we assume incompetence or greed on the part of doctors. That is part of the reason why doctors now recommend that smart people thinking about medicine should become nurse practitioners instead,
Citation: Smith, Timothy R. MD, PhD, MPH; Habib, Ali BA; Rosenow, Joshua M. MD; Nahed, Brian V. MD; Babu, Maya A. MD, MBA; Cybulski, George MD; Fessler, Richard MD, PhD; Batjer, H. Hunt MD; Heary, Robert F. MD, 'Defensive Medicine in Neurosurgery: Does State-Level Liability Risk Matter?', Neurosurgery: February 2015 - Volume 76 - Issue 2 - p 105–114 doi: 10.1227/NEU.0000000000000576






Comments