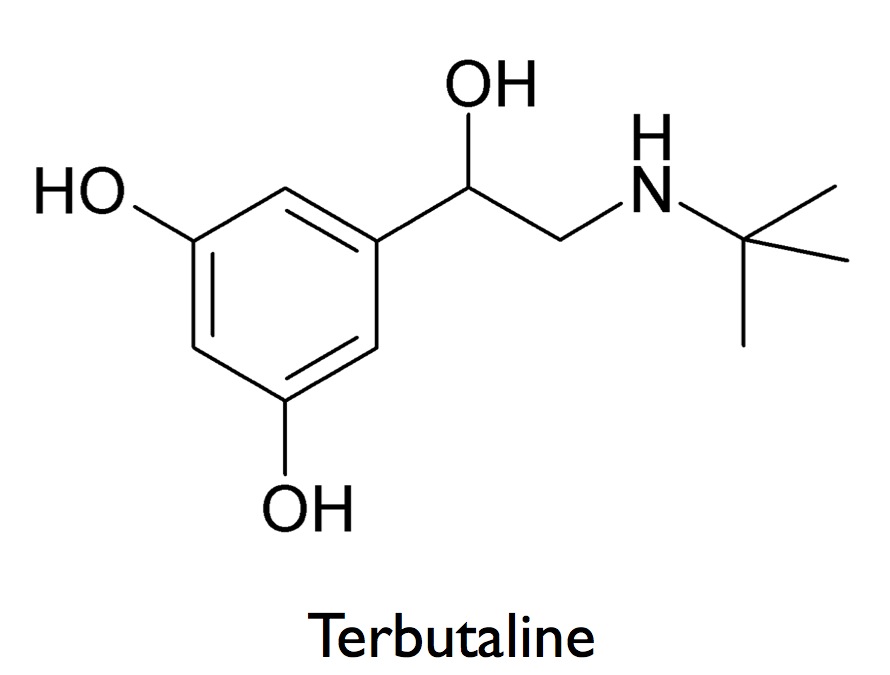
If you've ever had a severe asthma attack or gone into premature labor, there is a good chance you were given the drug terbutaline. Terbutaline can relax your involuntary smooth muscle when it's causing problems: in constricted airways during an asthma attack, or in the uterus during contractions. But if you've taken terbutaline, you've probably also noticed another effect: it can induce a pounding, racing heartbeat. How can one drug produce such opposite effects - relaxing smooth muscle in some parts of your body, while making your cardiac muscle work harder?
The answer is that terbutaline switches on a common information-processing module, called a signaling pathway, which gets used over and over in different cells to perform very different jobs. This information-processing module can be plugged into different cell types, where it will transmit signals from the environment outside the cell to the inside where the information is processed and acted upon. Because our cells use a common set of information-processing modules to carry out so many different jobs, it's easy for drugs that act on these modules to produce a wide range of side-effects.
Anatomy of an Information Processing Module
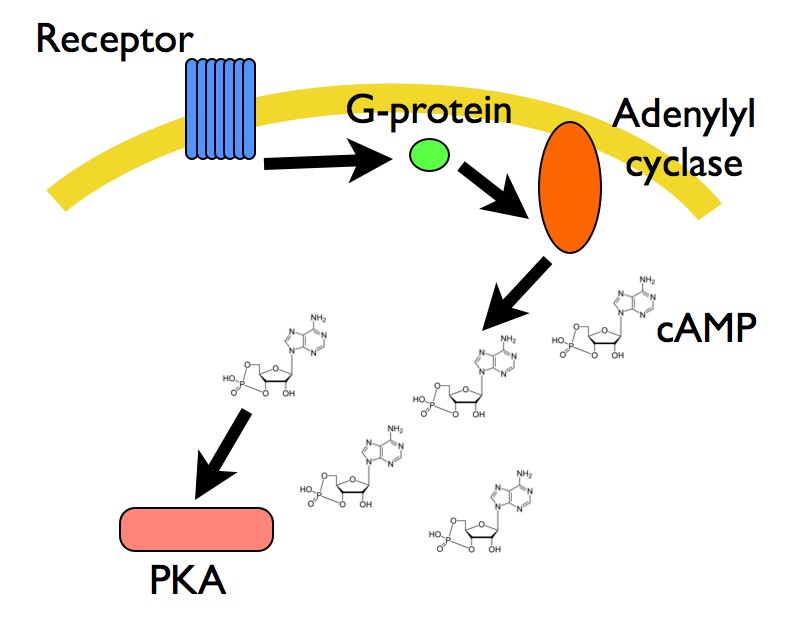
Let's take a look at one of these information-processing modules to see how terbutaline produces it's varied effects. Terbutaline closely resembles a hormone produced by your body, epinephrine (also known as adrenaline). Like epinephrine, terbutaline switches on a signaling pathway when it binds to a protein on the surface of a cell, a protein called a beta-adrenergic receptor. (Aficionados will know that there are several types of these receptors, and they have somewhat different roles in different tissues; terbutaline acts primarily on beta-2 receptors.) Once terbutaline binds the receptor, we get a cascade of chemical reactions like this:
1. The receptor activates a G-protein.
2. The G-protein turns on an enzyme called adenylyl cyclase.
3. Adenylyl cyclase produces a molecule called cAMP.
4. cAMP activates a protein called Protein Kinase A, or PKA.
5. PKA initiates many different downstream processes that produce a change in the cell (stronger muscle contractions in your heart, relaxation in your smooth muscle cells, and other effects in your gut and liver).
Like components in your computer, this pathway can be plugged into a variety of contexts. Connect the pathway to a different input at the top (say, a different receptor for a different hormone), and/or a different output at the bottom (make different PKA targets available), and voila: your information-processing module can do something else. Many of these pathways are very ancient modules, found in organisms from yeast to worms to flies to mammals. These modules have been so well conserved, that you can take take a human receptor, pop it into yeast, and that receptor will hook up with the yeast G-protein and start the cascade of chemical reations.
Why These Modules Work This Way
The module I outlined above may not make very much sense at first glance. Why does it work this way? There are two particularly important things this pathway does.
1. Just like a photomultiplier tube, which produces a detectable electric current from a single photon, this signaling pathway amplifies the intial signal. When one molecule of terbutaline turns on a receptor, that receptor turns on a G-protein, which turns on adenylyl cyclase. Adenylyl cyclase produces many molecules of cAMP, which can diffuse through the cell and activate all of the PKA around. If one active receptor produced only one molecule of cAMP, your signal would quickly fizzle out inside the cell (this is still true even when you allow for the fact that in a real cell you have hundreds of receptors getting activated by terbutaline). Molecules like cAMP are called second messsengers; they are 'messengers' slightly downstream of the activating signal which are produced in large numbers, large enough to get the message conveyed everywhere it needs to go.
2. This signaling pathway relays information spatially - from the surface of the cell, where the receptor sits, monitoring the environment, down into the guts of the cell, such as the nucleus, where genes get switched on and off, or internal calcium storage sites, which can produce a whole host of different effects in the cell (such as changing the electrical activity of heart muscle cells). Receptors and G-proteins hang out around the surface of the cell, but the small second messenger cAMP can diffuse away from the membrane, and over to the places where PKA can do its job.
Now that we've seen how these pathways work, we can come back to our original question about terbutaline: why are we set up to get such different responses from a drug that turns on beta-adrenergic receptors? We can find a clue by looking for the hormone that normally binds these beta-adrenergic receptors when externally-administered terbutaline is not around: epinephrine. Epinephrine is a major player in our fight-or-flight response: when trouble is brewing, our body gears up to survive the oncoming crisis by preparing to fight it out, or (more likely in my case) run away. To do either, we need plenty of oxygen and lots of blood flow (and obviously no labor contractions). Thus, epinephrine activates the information-processing module that gets our heart to pump more blood, and our airways to relax and open for more oxygen. The economy involved here is extremely elegant: instead of using a brand new signaling pathway for each different function, our cells use universal parts that help our bodies coordinate the complex responses we need in our day-to-day lives.





Comments