 Researchers have published the results of the largest prospective multicenter trial conducted of FDG-PET/CT in head and neck cancer, providing data on clinical decision-making.
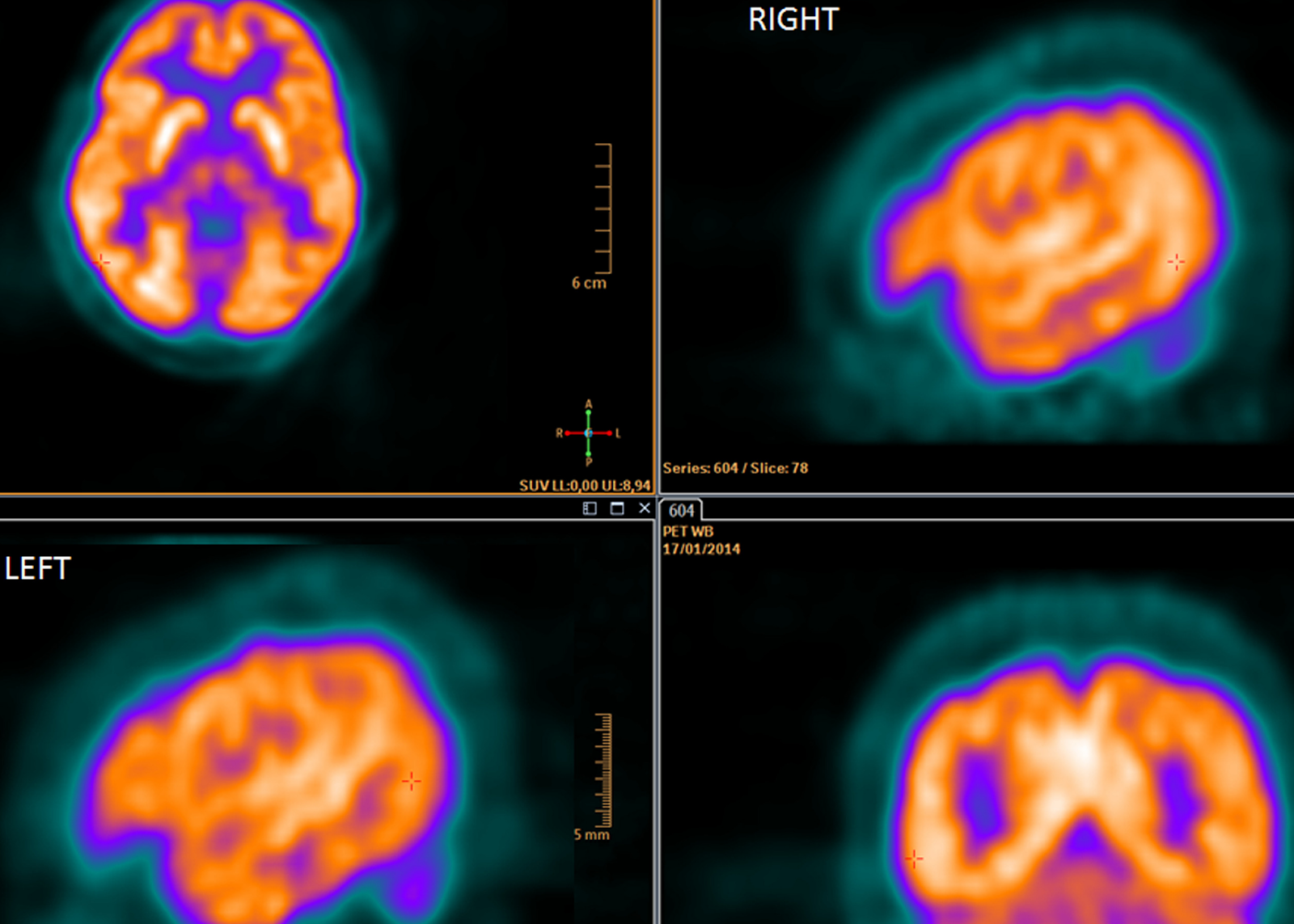
Researchers have published the results of the largest prospective multicenter trial conducted of FDG-PET/CT in head and neck cancer, providing data on clinical decision-making.The non-randomized phase two trial, ACRIN 6685, followed 287 patients with newly diagnosed stage T2 to T4 disease, all being considered for surgery when at least one side of the neck had no evidence of lymph node involvement based on a physical exam, preoperative MRI and/or a CT evaluation (clinically node-negative or cN0). It found that FDG-PET/CT imaging achieved a true negative in 94 percent of patients (by standardized uptake value (SUV) analysis), or 87 percent of patients (by visual assessment). The trial was designed and conducted by researchers in the ECOG-ACRIN Cancer Research Group with support from the National Cancer Institute, part of the National Institutes of Health.
"The information provided by FDG-PET/CT of the cN0 neck changed the surgical plan 22 percent of the time," said the study's principal investigator and lead author Val J. Lowe, MD, a nuclear medicine specialist at Mayo Clinic in Rochester, MN. "These findings suggest that FDG-PET/CT may assist the clinician in deciding on the best therapy for the clinically N0 neck in head and neck squamous cell carcinoma, possibly preventing patient morbidity and/or saving significant costs."
The reliability of FDG-PET/CT in detecting lymph node metastases in head and neck cancer is well proven and is reported to be cost-effective in staging patients with cN0 necks. Most of the data is single-institutional and retrospective. Surgeons often perform elective neck dissections in patients with cN0 necks at high risk for recurrence because clinical exam and structural imaging do not reliably identify all metastatic disease. This approach has been found to improve survival but may be associated with substantial complications for patients. The positive PET leads the surgeon to consider resection of nodal levels that might harbor occult metastatic disease.
The surgical plans were devised by the local surgeons on the basis of physical examination and CT and/or MRI results, but not PET/CT and thereafter formulated with the available PET/CT result. Both plans were collected prospectively with questionnaires. All data were anonymized to protect the identities of the participants. FDG-PET/CT scans and pathology findings were available for 270 cN0 neck sides from 212 participants. Pathology was randomly over-read by a central pathologist and all scans were reviewed by a team of central readers. For visual assessment, the negative predictive value (NPV) specific to the cN0 sides was 0.868 (95 percent CI, 0.803 to 0.925). For dichotomized maximum SUV, the NPVs specific to the nodal basins were 0.940 (95 percent CI, 0.928 to 0.952) and 0.937 (95 percent CI, 0.925 to 0.949) at prespecified cutoffs of 2.5 and 3.5, respectively. The optimal cutoff maximum SUV was determined to be 1.8, with an NPV of 0.942 (95 percent CI, 0.930 to 0.953).
The FDG-PET/CT-informed surgical treatment plan was changed in 51 of 237 participants (22 percent) compared with the PET/CT-blinded surgical plan. In 34 participants (12 percent), this led to planned dissection of additional nodal levels. In 12 participants (5 percent), this led to fewer planned dissected nodal levels. Negative PET/CT scans in N0 necks were true negative in 87 percent and false negative in 13 percent. "This trial is an excellent example of a means to implement personalized medicine in the setting of head and neck cancer management," said Dr. Stack. Research credit: ECOG-ACRIN Cancer Research Group / Journal of Clinical Oncology






Comments