A study of 338 patients with coronary artery disease has identified a gene expression profile associated with an elevated risk of cardiovascular death. Used with other indicators such as biochemical markers and family history, the profile – based on a simple blood test – may help identify patients who could benefit from personalized treatment and counseling designed to address risk factors.
Researchers found the risk signature by comparing gene expression profiles in 31 study subjects who died of cardiovascular causes against the profiles of living members of the study group. Twenty-five of the 31 deaths occurred in the group with the high-risk profile, though coronary deaths were also recorded among the lower risk members of the study group. All of the patients studied had coronary artery disease (CAD), and about one in five had suffered a heart attack prior to the study.
Researchers from the Georgia Institute of Technology, Emory University and Princeton University participated in the study, which obtained gene expression profiles from blood samples taken from patients undergoing cardiac catheterization at Emory University clinics in Atlanta. The results are scheduled to be published in the open-access journal Genome Medicine on May 29, 2014.
"We envision that with our gene expression-based marker, plus some biochemical markers, genotype information and family history, we could produce a tiered evaluation of people's risks of adverse coronary events," said Gregory Gibson, director of the Center for Integrative Genomics at Georgia Tech and one of the study's senior authors. "This could lead to a personalized medicine approach for people recovering from heart attack or coronary artery bypass grafting."
Coronary artery disease is the leading cause of death for both men and women in the United States. Manifested in the narrowing of blood vessels through the buildup of plaque, CAD sets the stage for heart attacks and long-term heart failure.
As many as half of Americans over the age of 50 suffer from CAD to some extent, so the researchers wondered if they could single out those with the highest risk of death. From a cohort of more than 3,000 persons known as the Emory Cardiovascular Biobank (EmCD), they selected two groups of patients for extensive gene expression analysis based on blood samples.
After following the patients for as long as five years, the researchers examined gene expression patterns in a total of 31 persons from the study group who had suffered coronary deaths. Comparing these patterns against those of other study subjects revealed a pattern in which genes affecting inflammation were up-regulated, while genes affecting T-lymphocytes were down-regulated.
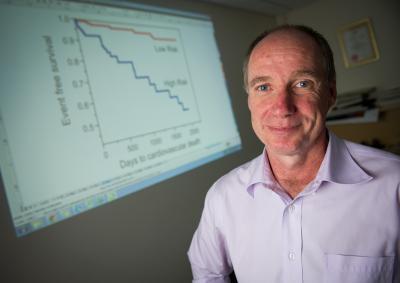
Georgia Tech Professor Gregory Gibson poses with a chart showing death rate differentials between groups of coronary artery disease patients identified with a new gene expression profile.
(Photo Credit: Georgia Tech Photo: Rob Felt)
The patients studied ranged in age from 51 to 73, were mostly Caucasian, and 65 percent male. Seventy percent of the subjects had significant CAD, and 18 percent were experiencing an acute myocardial infarction when blood samples were taken. Gene expression was analyzed using microarrays and two different normalization procedures to control for technical and biological covariates. Whole genome genotyping was used to support comparative genome-wide association studies of gene expression. Two phases of the study were conducted independently with the two different groups, and produced similar results.
"What's new in this research is the recognition that this risk pathway exists and that it relates to particular aspects of immune system functions that include T-cell signaling," said Gibson, who is also a professor in Georgia Tech's School of Biology. "We went beyond the signature of coronary artery disease to really provide a signature for adverse outcomes in that high-risk population."
The pattern, said Gibson, doesn't indicate the causes of the disease. The researchers would now like to expand the study to include a larger group of patients and learn more about what causes the disease. They'd also like to know whether the risks can be reversed through diet, exercise or drug therapy.
Cardiologist Arshed Quyyumi, the paper's other senior author, directs Emory University's Clinical Cardiovascular Research Center and created the Biobank five years ago to facilitate cardiovascular research. He says that identifying patients at highest risk could help encourage their compliance with treatment programs, and prioritize introduction of newer therapeutics, such as cholesterol lowering medications like PCSK9 inhibitors.
"A number of patients with CAD are currently not maximally treated," said Quyyumi, who is a professor in Emory's School of Medicine. "In those that appear to have been prescribed adequate medication, a significant proportion of subjects are non-compliant with their medications. Thus, knowledge of a high risk genetic profile in a patient can prompt both the patient and physician to maximize currently available medications and improve patient compliance."
Approximately 15,000 genes are expressed in human blood, but analyzing them is not as daunting as it sounds. Most of the gene expression is correlated, so there may be only a few dozen independent measurements that can be related to disease states, Gibson said. In the study, researchers identified nine "axes" that represented specific biological pathways to disease. Two of them were relevant to the high-risk profile.
Gibson believes identifying the high-risk signatures in CAD patients may lead to opportunities for improving their health.
"Our dream would be a hand-held device that would allow patients to take a droplet of blood, much like diabetics do today, and obtain an evaluation of these transcripts that they could track at home," he said. "If we can use this information to help people adopt healthier behaviors, it will be very positive."






Comments