“Wow, there’s a lot of plaques of fat. I need to stop eating French fries.”
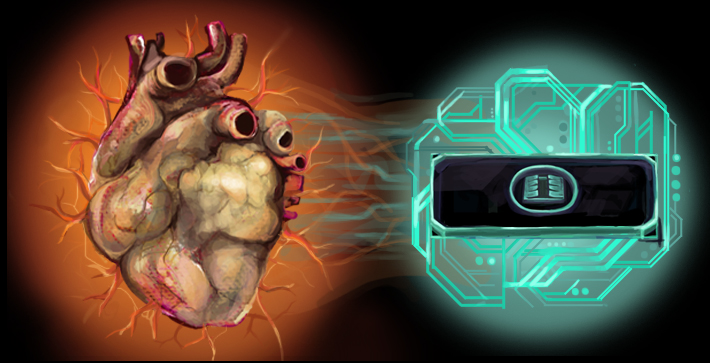
Nine years later, the “cardiac tissue engineer,” is trying to re-create the human heart on a chip.
Without the arterial plaque, of course, but one that perfectly re-creates the cardiac cells and mechanical forces of the human heart. A slice of glass, the size of a quarter, tiered with four layers, including real pumping cardiac cells and the sticky fibronectin that gives them shape. It’s not exactly a computer chip, but it’s fabricated in much the same way as one. If all goes well, these “organs-on-chip” may mean a rather dramatic testing ground for new drugs, as well as a miniature lab for personalized pharmaceutical testing.
Credit: USC
It's good timing. Heart disease claimed more American lives in 2013 than the first and second world wars did combined.
Future treatments might still involve ACE inhibitors and a Beta blocker, but they would first be tested on your heart cells without ever entering your body. Using a technique of converting your own skin cells to stem cells and from there to heart cells, the newly harvested tissue might be tested in a 2.5-cm laboratory similar to McCain’s.
But the potential for the pharmaceutical industry is even more astonishing. 95 percent of all drugs fail in humans, proving either too toxic or too ineffective. It’s one reason that the average cost of a drug approved by the U.S. Food and Drug Administration is around $5 billion. That cost and failure rate, coupled with a short window before drugs go generic, are why new treatments have to be so successful.
At present, if Pfizer or Eli Lilly wants to test a new heart disease drug, there are two options: animal testing, primarily in mice, or testing cell cultures in a petri dish. But both have obvious drawbacks. Mice may be complex biological organisms, but they’re not humans — recent studies show it’s not a good predictor of what works in humans. And haphazard cell cultures in a dish isn’t exactly the “home sweet home” cell architecture they might find in a working human heart.
For example, let’s consider that human heart: millions of cardiac myocytes — heart muscle cells — contracting in one glorious, simultaneous symphony. Throwing them in a petri dish allows for none of these mechanical forces — all the stretching, squishing, pulling real heart cells must respond to.
“[With organs-on-chip] you can fail fast and fail cheap,” McCain said. “If something’s going to interact poorly in the human heart, you want to be able to catch it early.”
Muscles and myocytes
McCain’s heart-on-chip promises not only to replicate the precise horizontal alignment of myocytes — physically and electrically bound in cozy horizontal rows — but the very stiffness and shape found inside humans.
McCain likes muscles. She thinks about them as she does spin class at 6:30 in the evening. She wonders how efficiently her heart is pumping blood and whether her tiny chip can do the same (unlike her real heart, the chip can measure that).
The real human heart has lots of collagen. While at Harvard University, McCain had the idea of replicating that Jell-O-like texture in her heart-on-a-chip. So she started growing myocytes on soft gelatin hydrogel instead of silicone rubber. Now the myocytes are much happier: They end up living for a month rather than a week — a rather important thing if you want to test the longer term effects of drugs.
“Mechanical forces,” she noted, “have not been well studied in the human heart. For example, the stiffness affects how well the myocytes contract and couple together in the heart.”
One of the big challenges of heart disease is understanding all the underlying mechanisms that cause it. According to McCain, there’s just so much happening at once: The cells are exploding in size, the heart becomes stiffer and the rows of cells become misaligned. Which factor is the most significant? McCain is hoping to model these effects individually, possibly finding new insights into therapeutic drugs.
McCain, who as a child dreamed of being a Disney animator, has long forgotten about drawing cartoon mice. But she’s still very proud of her “home movies” — beating myocytes captured at hundreds of frames a second under a fluorescent microscope.
For her, watching thousands of myocyctes beating in perfect unison, that’s as cinematic as any fantasy from Neverland or King Triton’s kingdom or 100-Acre Woods.
After all, it’s the heart at its most fundamental level.
Source: USC






Comments