The findings indicate that the independence and sense of autonomy that doctors have in small practices may provide some protection against symptoms of burnout. Whether that feeling of autonomy will last as health care becomes more centralized is another issue, but for now 13.5 percent reporting being burned out in smaller practices versus 54.4 percent at large ones.
Physician burnout is a major concern for the healthcare industry, according to the American Council on Science and Health. It is associated with low job satisfaction, reduced productivity among physicians, and may negatively impact quality of care.
Multiple national surveys suggest that more than half of all physicians report symptoms of burnout but analyses of physician burnout has focused primarily on hospital settings or large primary care practices in urban locations. The researchers say that this is the first study that examines the prevalence of burnout among physicians in small independent primary practices. Despite declines in the number of small practices in the United States, primarily due to market forces driving consolidation, close to 70 percent of all primary care office visits occur in small practice settings, according to the American Medical Association.
Researchers examined data collected from 235 physicians practicing in 174 small practices in New York City. The rate of provider reported burnout was 13.5 percent, compared to the 2014 national rate of 54.4 percent. A 2013 meta-analysis of physician surveys conducted in the United States and Europe found that lower burnout rates were associated with greater perceived autonomy, a quality and safety culture at work, effective coping skills, and less work-life conflict.
"Burnout is about the practice culture and infrastructure in which primary care doctors work. So the obvious question is: what is it about the work environment that results in low burnout rates in small practices?" said Donna Shelley, MD, professor of Population Health and Medicine at NYU School of Medicine, and the study's senior author. "It's important to study the group that's NOT showing high burnout to help us create environments that foster lower burnout rates. The good news is that a culture and systems can be changed to support primary care doctors in a way that would reduce the factors that are leading to burnout."
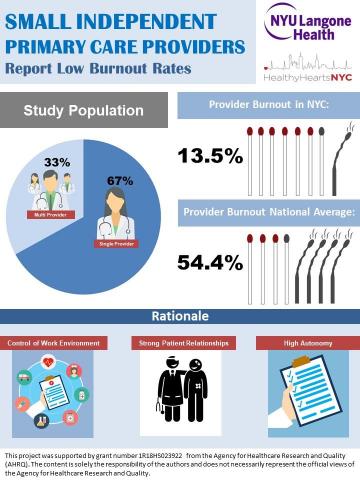
Credit: Department of Population Health, NYU Langone Health
How the Study Was Conducted
Researchers analyzed data as part of the HealthyHearts NYC (HHNYC) trial, which is funded by the Agency for Healthcare Research and Quality's (AHRQ) EvidenceNOW national initiative. AHRQ is a division of the U.S. Department of Health and Human Services. The HHNYC trial evaluates how practice coaching or facilitation helps SIPs adopt clinical guidelines for the treatment and prevention of cardiovascular disease.
Each physician answered a multiple choice question with response options indicating various levels of burnout. Options ranged from no symptoms of burnout, to feeling completely burned out and questioning whether or not to continue practicing medicine. The question was validated against the Maslach Burnout Inventory, a nationally recognized measure that identifies occupational burnout. Physician respondents were categorized as burned out if they checked one of the last three options in the multiple choice question.
As part of the HHNYC trial, physician respondents were also asked a number of questions about the culture of their practices. The tool used specifically measures "adaptive reserve," or a culture where individuals have opportunities for growth, and the ability to learn from mistakes by talking and listening to each. Physicians that described this kind of culture in their practice reported lower levels of burnout. According to Dr. Shelley, practices where employees feel that they are included in decisions and have control over their work environment are referred to as having 'high adaptive reserve."
The authors list a number of the study's limitations. Since the findings are representative of physicians working in small practices in New York City, the study does not capture burnout rates in other cities across the country. It is also possible that the researchers underestimated the number of hours worked by physicians, since hours worked is associated with burnout. Shelley also cited the lack of data linking physician burnout to patient outcomes.
It's not simply that physicians working in solo or small practices face fewer challenges. Burnout rates are lower, but the paperwork is still overwhelming and that means many of these practices are struggling financially. Many of these physicians are on call all of the time.





Comments