Heart disease is the world's leading cause of death, but recent advances in science and medicine have improved the chances of surviving a heart attack. In the United States alone, nearly one million people have survived an attack, but are living with heart failure—a chronic condition in which the heart, having lost muscle during the attack, does not beat at full capacity.
Scientists have been look at cellular reprogramming as a way to regenerate this damaged heart muscle. And it works. Scientists can transform skin cells into cells that closely resemble beating heart cells but it's complicated and the transformation is often incomplete.
Now, scientists at the Gladstone Institutes have devised a new method that allows for the more efficient - and more complete — reprogramming of skin cells into cells that are virtually indistinguishable from heart muscle cells.
The reprogramming of skin cells into heart cells, pioneered by Gladstone Investigator Deepak Srivastava, MD, requires the insertion of several genetic factors to spur the reprogramming process. However, scientists have recognized potential problems with scaling this gene-based method into successful therapies. Gladstone Senior Investigator Sheng Ding, PhD, has taken a somewhat different approach.
"Scientists have previously shown that the insertion of between four and seven genetic factors can result in a skin cell being directly reprogrammed into a beating heart cell," explained Ding, the paper's senior author and a professor of pharmaceutical chemistry at UC San Francisco, with which Gladstone is affiliated. "But in my lab, we set out to see if we could perform a similar transformation by eliminating—or at least reducing—the reliance on this type of genetic manipulation."
To that effect, the research team used skin cells extracted from adult mice to screen for chemical compounds, so-called 'small molecules,' that could replace the genetic factors. Dr. Ding and his research team have previously harnessed the power of small molecules to reprogram skin cells into neurons and, more recently, insulin-producing pancreas cells. They reasoned that a similar technique could be used to do the same with heart cells.
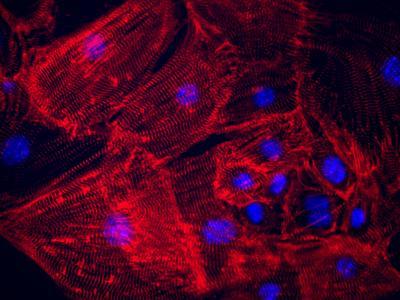
Beating heart cells have been reprogrammed from skin cells using a combination of a chemical cocktail and just one genetic factor (Oct. 4). Reducing scientists' reliance on gene-based reprogramming approaches paves the way for pharmaceutical-based approaches that could more easily translate into successful therapies. Credit: Haixia Wang/Gladstone Institutes
"After testing various combinations of small molecules, we narrowed down the list to a four-molecule 'cocktail,' which we called SPCF, that could guide the skin cells into becoming more like heart cells," said Gladstone Postdoctoral Scholar Haixia Wang, PhD, the paper's lead author. "These newly reprogramed cells exhibited some of the twitching and contracting normally seen in mature heart cells, but the transformation wasn't entirely complete."
So, Drs. Ding and Wang decided to add one genetic factor, called Oct4, to the small molecule cocktail. And by doing so, the research team was able to generate a completely reprogrammed beating heart cell.
"Once we added Oct4 to the mix, we observed clusters of contracting cells after a period of just 20 days," explained Dr. Ding. "Remarkably, additional analysis revealed that these cells showed the same patterns of gene activation and electric signaling patterns normally seen in the ventricles of the heart."
Dr. Ding and his team believe that these results may point to a more desirable method for reprogramming, as ventricular heart cells are the type of cells typically lost during a heart attack. These findings give the team newfound optimism that the research is well on its way towards an entirely pharmaceutical-based method to regrow heart muscle.
"The fact that the combination of Oct4 and small molecules appears to generate beating heart cells in an accelerated fashion is encouraging," said Joseph Wu, MD, PhD, Director of the Stanford Cardiovascular Institute, who was not involved in this study. "Future advances by Dr. Ding and others will likely focus on improving the efficiency of conversion as well as duplicating the data in adult human cells."






Comments