According to the American Cancer Society (ACS) lung cancer is the leading cause of cancer deaths for both men and women. Deaths from lung cancer exceed those from breast, prostate and colon cancers combined. In 2008 the ACS estimates 162,000 lung cancer deaths in the United States. Currently, after a diagnosis of lung cancer only about 40 percent of people remain alive after the first year.
These statistics are severe due to the virulent nature of lung cancer in general, but also due to the drastic treatment that follows its diagnosis. “The standard of care for patients with this particular disease is a lobectomy, or surgical removal of the entire lobe of the lung, says AGH radiation oncologist Dr. Athanasios Colonias. “Many patients, however, are considered high-risk for this procedure due to cardiopulmonary complications or other co-morbidities.”
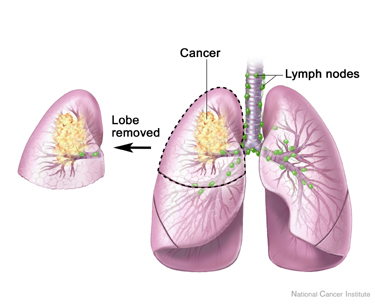
Traditional treatment for lung cancer includes the surgical removal of an entire lobe of the affected lung, causing severe cardiopulmonary complications. Photo credit: Siteman Cancer Center, Washington University School of Medicine
That is all about to change. By introducing the intraoperative 1251 Vicryl (R) mesh brachyotherapy, AGH methods could save countless lives otherwise taken by lung cancer. What this method entails is removal of only the cancerous tissue of the lung (sublobar resection) and then enveloping the surgical site with a mesh material that is embedded with radioactive seeds which emit a low dose radiation over a prolonged period of time.
“Sublobar wedge resection is a more tolerable approach, but one that carries a much higher chance of cancer recurrance,” clarifies Colonias.
This combination of surgical removal with radiation provides a much more effective and safe procedure than by previous methods.
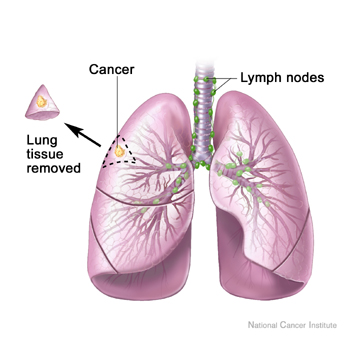
With advanced treatment, only the cancerous tissue is removed and mesh embedded with radioactive seeds is placed over the surgery site and emits radiation to destroy any remaining cancer cells. Photo credit: Siteman Cancer Center, Washington University School of Medicine
The AGH study, investigated over 12 years, looked at 145 high risk cases of stage 1 non-small cell lung cancer. Their procedure included sublobar resection and induction of the mesh brachytherapy. After a follow-up period of 38 months, only 6 of the cases showed a recurrence of cancer. This 4.1 percent recurrence rate was significantly lower compared to the 20 percent recurrence rate with just the sublobar resection based on previous studies.
“Our study suggests that when intraoperative 1251 Vicryl (R) mesh brachytherapy is added to sublobar resection, the local treatment failure rate is substantially reduced,” says Colonias.
Data from this study as well as supporting studies suggests a high success rate for this treatment, which could mean that this technique could also be utilized more fully in the future to treat a wide range of cancers, as well as maintaining a higher quality of life for patients.





Comments