It has been almost 400 years since the publication of Exercitatio anatomica de motu cordis et sanguinis in animalibus ("On The Motion Of The Heart And Blood In Animals") by the British physician William Harvey, which accurately described the circulation of the blood around the body, and we are still discovering the secrets of the circulatory system and its contents.
This is especially relevant when leveraging the circulatory system’s contents for clinical applications, such as prenatal testing.
The presence of circulating fetal DNA in maternal blood was first reported in the mid-1990s,and this discovery has led to unprecedented rapid and dramatic improvements in the prenatal testing market. The development of non-invasive prenatal testing (NIPT) offers women, for the first time, a method to screen for fetal chromosome abnormalities that is both safe – only a blood draw is required – and also highly accurate.
Around four million babies are born in the United States every year. The majority of pregnant women undergo serum screening, which is a blood test that measures circulating levels of specific hormones, along with ultrasound screening. Unfortunately, this type of screening is not very accurate – it only catches about 83% of abnormal pregnancies and has a high rate of false positives (~5% of all tests are false positives); women with positive results are advised to have an invasive diagnostic test for confirmation.
This means a lot of women with healthy, normal pregnancies are getting inaccurate screening results, causing them undue stress and anxiety about whether something is wrong, and leading to unnecessary invasive testing. Invasive tests like amniocentesis or chorionic villus sampling (CVS) are highly accurate but they come with a small risk of miscarriage,and many women want to avoid any kind of invasive procedure, especially when pregnant. The introduction of NIPT has dramatically improved detection rates and, importantly,significantly reduced false positive rates.
This means that more affected pregnancies are detected with NIPT, and fewer women will be faced with having to decide whether or not they should have potentially unnecessary invasive testing. A study published in 2013 found that the introduction of NIPT could result in a reduction in invasive procedures by more than 95%, compared with the older screening methods.
NIPT methods involve isolating cell-free DNA – some of which is fetal – from the plasma layer of a pregnant woman’s blood, amplifying it and measuring it with a sequencer. There are two main types of NIPT methods that are commercially available, counting methods and the single-nucleotide polymorphism(SNP)-based method, with each using a different type of information that can be derived from the DNA.
The counting method counts the number of DNA sequences from the chromosome-of-interest and compares this to the number of sequences from a reference chromosome which is known to have two copies. For a fetus with Down syndrome, who has three copies of chromosome 21 instead of two, the amount of DNA from chromosome 21 would be increased by 50%.
On average, around 10% of the DNA in maternal plasma originates from the fetus, so for the counting method to detect fetal Down syndrome, it must detect the ~5% increase in chromosome 21 DNA in the plasma sample.
The SNP-based method, on the other hand, is a more sophisticated approach that measures the DNA at a few thousand SNPs (individual genetic base pairs that often differ from person to person) per chromosome. As each person inherits one chromosome from each of their parents, the SNP patterns resulting from the possible genotypes of the fetus can be predicted at each SNP based on the genotype of one or both parents.When a fetus inherits an abnormal number of chromosomes, there will be an abnormal fetal SNP pattern in the mother’s blood sample at the chromosome with an extra or missing copy.
This method looks at the mother’s DNA (and father’s, if available), predicts all of the possible fetal genotypes, and then applies a computer algorithm to compare the predicted genotypes to the genotype that was actually observed in the mother’s plasma to find the one that matches best. Additionally, the use of SNPs allows the use of a number of quality metrics to ensure that samples – even those with a very low fraction of fetal DNA – are called correctly. 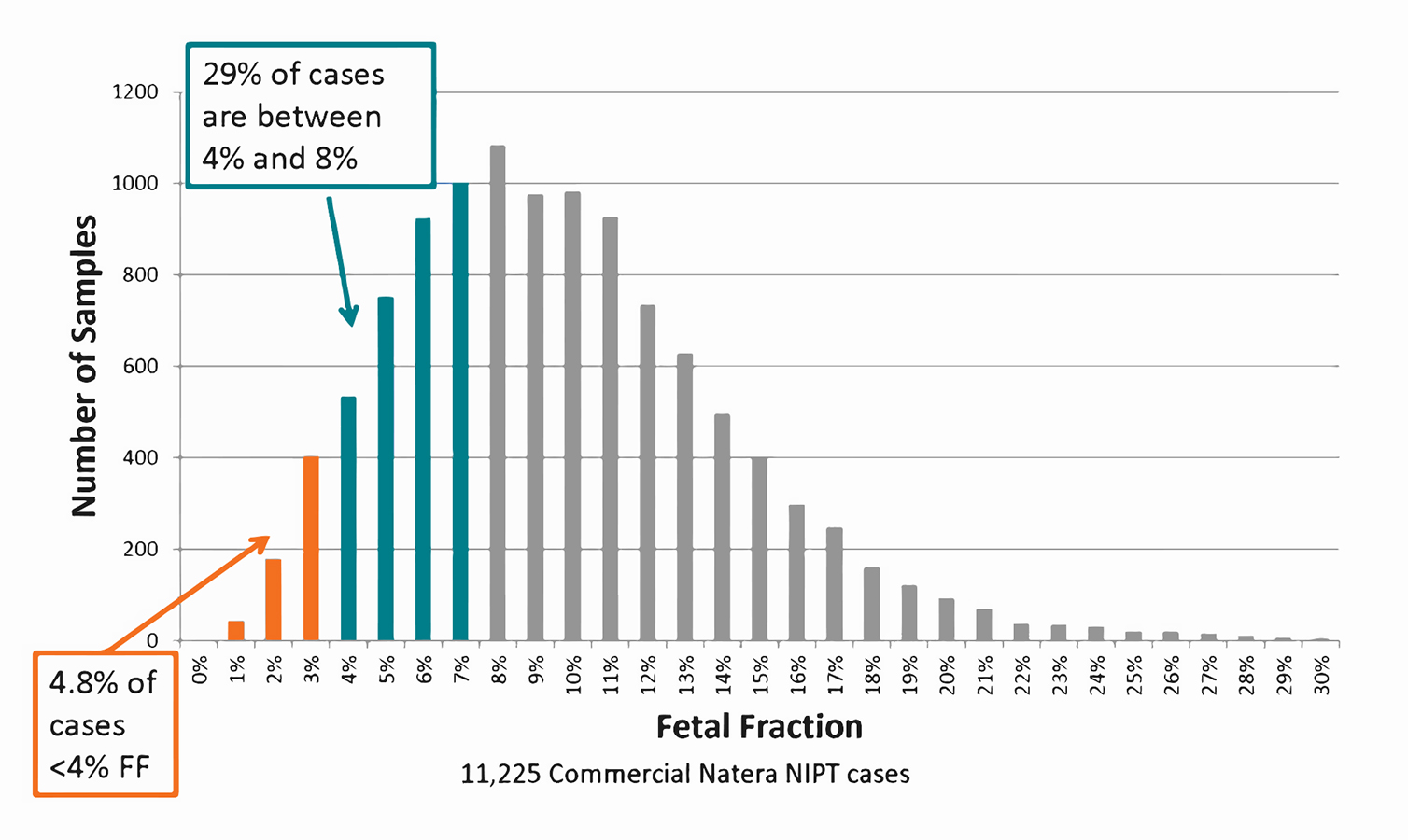
Up to 1/3 of all NIPT cases have <8% fetal fraction, which is often associated with decreased sensitivity. Credit: Natera
Both NIPT methods screen for fetal genetic disorders that arise from extra or missing chromosomes, such as Down syndrome, Edwards syndrome, and Patau syndrome, along with fetal sex and sex chromosomal disorders such as Turner syndrome and Klinefelter syndrome. Around 1 in 200 pregnancies is affected by one of these syndromes. NIPT can also detect conditions where a small part of the chromosome is missing, called a micro deletion,such as 22q11.2 deletion syndrome (DS, often called Di-George Syndrome); the SNP-based method performs considerably better than counting methods on these smaller chromosome regions.
In addition, the SNP-based approach can uniquely detect twins and triploidy (where the fetus has an extra copy of all of the chromosomes).
Thanks to the additional quality metrics, the SNP-based method can be carried out as early as nine weeks of gestation, while tests using the counting method are available from ten weeks onwards.
Screening for a wide range of chromosomal abnormalities early in pregnancy can lead to better pregnancy management, including earlier therapeutic intervention and the prediction and possible prevention of pregnancy complications. For example, fetal triploidy can cause serious maternal complications such as severe early-onset preeclampsia and choriocarcinoma (cancer in the womb).
Finding out your child may have a microdeletion condition such as 22q11.2 DS allows for appropriate birth preparations in case of potential birth complications, along with early therapeutic interventions that can improve their chances of leading a healthy life. Detection of sex chromosome aneuploidies, which are often not detected until puberty or adulthood when trying to conceive, allows early therapeutic treatment with hormones which, according to a recent study, may improve neuro-developmental function in children diagnosed with Klinefelter syndrome.
The expansion of the prenatal testing market to include NIPT offers pregnant women a safe and accurate method of screening for a variety of fetal abnormalities, helping to alleviate anxiety and allowing them to make informed decisions regarding their pregnancy.
All of this, from a few drops of blood.






Comments