Helicobacter is presumed to be present in about 50% of the world's population upper gastrointestinal tract, while fully 80% of individuals harboring this organism are asymptomatic.
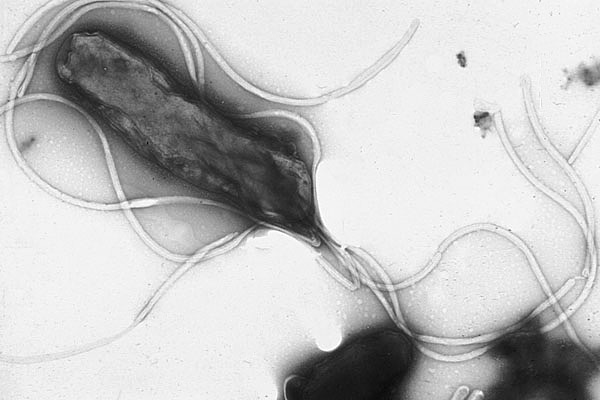
Furthermore, Helicobacter has been associated with the development of stomach cancers.
Now we get to the difficult bit.
Helicobacter has been declining in many developed countries, which has been associated with an increase in esophageal adenocarcinomas. This isn't merely a speculative connection.
http://www.ncbi.nlm.nih.gov/pubmed/20399210
http://www.ncbi.nlm.nih.gov/pubmed/19138977
http://www.sciencedaily.com/releases/2008/10/081006092511.htm
As a result, one fundamental perception is changing, as it relates to the germ theory of disease. It appears that not all microbes that may be pathogenic in one sense are necessarily uniformly pathogenic. In other words, while a microbe may cause some problems in susceptible individuals, it may also confer benefit to others (1). In short, the notion that microbes are only associated with disease outcomes isn't necessarily correct.
As a result, their evolution is inextricably linked to human evolution, as well as to human disease. “Our microbes are a part of human physiology… as much a part… as our liver, or our kidneys, or our heart,” Blaser commented. “They are a metabolic compartment or a series of metabolic compartments in the human body and how they behave and… their characteristics are relevant to health and disease.”This is causing a reevaluation of the differences between short-term infections and persistent colonization, even for the same microbe. What may appear to be a beneficial eradication of the problem microbe, may create other problems that are worse than the original.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1479565/pdf/7400699.pdf
In short, we may have to shift our disease paradigm to a more complex understanding that these microbial relationships may have a biological cost/benefit extending beyond simple "good" or "bad" assessments. Essentially the human body, in this example, is simply the environment in which these microbes live, exploiting and modifying their "world" to best suit their own needs. In the same way we see organisms modifying their environments in the macro-world, we are the environment being modified in the micro-world.
As a result, the viewpoint of good and bad must be replaced with what works and what doesn't. Simply viewing this intricate ecosystem as being an "us versus them" scenario is wrong.
From a purely speculative perspective, it appears that we may be experiencing microbes in various stages of adaptation with respect to our bodies. Some manage the environment well and help us survive. Some may be harmful or beneficial, depending on circumstances. Even our notion of disease may simply be the result of new "colonizers" entering a territory and engaging in chemical warfare with those already present.
Clearly there are some, including viruses, that have no fundamental connection to this human environment and simply exploit the available resources before they move on, or are eradicated. In any case, science is beginning to recognize that our relationship with microbes is significantly more complex than previously thought, and that life isn't merely a metaphorical web, but is inextricably linked; organism to organism, in a complex relationship of environments and ecosystems that are exploited for diverse purposes.
For more on the history of Helicobacter:
http://www.plosgenetics.org/article/info%3Adoi%2F10.1371%2Fjournal.pgen.0020120
===========================================
(1) Helicobacter as been inversely associated with childhood asthma, type II diabetes, and even obesity.
In addition, H. pylori affects gastric hormones that have a role in energy homeostasis, such as leptin and ghrelin; a link between its disappearance and the increasing prevalence of metabolic syndrome, type II diabetes and obesity has also been postulated (Blaser&Atherton, 2004).
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1618379/




Comments