The authors claim such particulate matter, 1/40th the width of even a human hair, can damage sleep. Larger particles are of course a problem. PM 10 is what is causing all of the problems in China but America has the cleanest air in the world. Claims about PM2.5 instead rely on unconfirmed "hormesis", the opposite of the dose makes the poison, which believes that normal or high amount of something are harmless but tiny amounts can cause damage.
In the EPA of recent years, where the drive was on to throw out toxicology and to simply accept claims on surveys published in epidemiology papers, this was gaining traction. But a new administration has declared that evidence must be presented, regulations can't be implemented by believing a epidemiological claim, as Linda Birnbaum, director of the National Institute for Environmental Health Sciences, wants to do, and then telling government scientists to go find a biological mechanism to affirm it. And using grey literature that hasn't been through peer review.
A new presentation is firmly in the epidemiological correlation camp and not science. Researchers analyzed data from 1,863 participants (average age 68) in the Multi-Ethnic Study of Atherosclerosis (MESA) who also enrolled in both MESA's Sleep and Air Pollution studies. The researchers looked at nitrogen dioxide (NO2), which is related to traffic congestion, and PM2.5. They then mapped the survey results to air pollution measurements gathered from MESA Air and Environmental Protection Agency monitoring sites in six U.S. cities. Some statistical manipulation layer and they estimated air pollution exposures at each participant's home at two time points: one year and five years.
Wrist actigraphy, which measures small movements, provided detailed estimates of sleep and wake patterns over seven consecutive days. This was used to calculate "sleep efficiency"--a measure of the percentage of time in bed spent asleep vs. awake. Researchers found that the sleep efficiency of the lowest 25 percent of participants was 88 percent or less. The research team studied if pollution exposures differed among those in this low sleep efficiency group.
Credit: ATS 2017
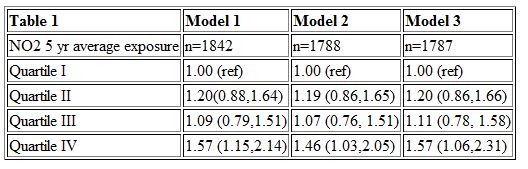
The population was divided into "fourths" according to levels of pollution. The quarter of those who experienced the highest levels of pollution was compared to the quarter with the lowest levels. Using that, they then declared that this air pollution causes upper airway irritation, swelling and congestion, and affects the central nervous system and brain areas that control breathing patterns and sleep.
They factored out people with sleep apnea, obesity, those who smoke, etc. It still has too many confounders to count. Old people didn't sleep well 200 years ago either, and only a few other characteristics of the participants are known. They still declared that group with the highest levels of NO2 over five years had an almost 60 percent increased likelihood of having low sleep efficiency compared to those with the lowest NO2 levels. The group with the highest exposures to small particulates (PM2.5) had a nearly 50 percent increased likelihood of having low sleep efficiency.
EPA is scrambling to justify their much larger size, and inventing new problems to solve is the best way to do it, but that won't protect the health of Americans. NO2 levels have plummeted, our air has never been cleaner, and despite claims by bureaucrats, PM2.5 has never caused an acute death during the entire existence of the EPA.
SOURCE: ATS 2017 International Conference Abstract 11211 Relationship of Air Pollution to Sleep Disruption: The Multi-Ethnic Study of Atherosclerosis (MESA) Sleep and MESA-Air Studies, M.E. Billings, D.R. Gold, P.J. Leary, A. Szpiro, C.P. Aaro, J.D. Kaufman, S.S. Redline






Comments