But you should understand how numbers can be manipulated. There is also conspiracy theory that political activists are exaggerating or underestimating the disease in an election year.
They can both argue their case because the commonly reported case fatality ratio (CFR) doesn't inspire confidence. A better solution might be the symptomatic case fatality ratio (sCFR) and the infection fatality ratio (IFR), according to a computational model of the dynamics of transmission of SARS-CoV-2 along with COVID-19 associated mortality.
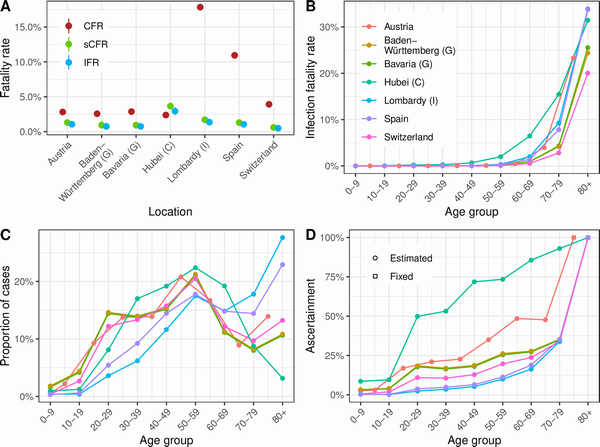
(A) CFR, sCFR, and IFR estimates by geographic location. (B) IFR estimates by age group and location (for Austria, the estimates are adapted to the available age groups from 0–4 to 75+ years). (C) Proportion of cases ascertained by age group and location (color code as for panel B). (D) Distribution of reported cases by age group by location (color code as for panel B). CFR, case–fatality ratio; C, China; G, Germany; I, Italy; IFR, infection–fatality ratio; sCFR, symptomatic case–fatality ratio. Credit: https://doi.org/10.1371/journal.pmed.1003189.g004
The model took into account the delay between infection and death, the increased diagnosis of disease in people with severe symptoms, and stratified data by age.
The researchers applied the model to Hubei province (China), Austria, Bavaria (Germany), Baden- Württemberg (Germany), Lombardy (Italy), Spain and Switzerland. In Hubei, the calculated IFR was 2.9% (95% credible interval [CrI] 2.4-3.5) while the CFR was 2.4%. In Europe, estimates of the IFR ranged from 0.5 (95% CrI 0.4-0.6) to 1.4% (95% CrI: 1.1-1.6) while the CFR ranged from 3.9% to 17.8%. Overall, estimates of sCFR and IFR were similar to each other and varied less geographically than the CFR.
"The CFR is not a good predictor of overall mortality from SARS-CoV-2 and should not be used for evaluation of policy or comparison across settings," the authors say. "The sCFR and IFR, adjusted for [the right biases], are measures that can be used to improve and monitor clinical and public health strategies to reduce the deaths from SARS-CoV-2 infection."





Comments