The following table gives examples of commonly used cytotoxic drugs, when they were first used, and how likely they are to cause vomiting:
| Drug | Year approved | Emetogenicity potential** |
| Adriamycin | 1974 | High |
| Cisplatin | 1978 | High |
| Vincristine | 1963 | Minimal |
| Cyclophosphamide | 1959 | High |
| Carboplatin | 1989 | Moderate |
| Methotrexate | 1953 | High |
| Taxotere | 1996 | Low |
| Etoposide | 1983 | Low |
| Fluorouracil | 1957 | Low |
** Emetogenicity potential (without antiemetic therapy):
High 90+%, Medium 30-90%, Low 10-30% Minimal <10%
Cytotoxic drugs, which are toxic to all cells, operate under the principle that cancer cells, which divide faster than non-cancerous cells faster, will be selectively killed . But, this selectivity is limited, so both normal and cancer cells are exposed to poisons. As barbaric as this sounds, it remains the foundation of most cancer treatments. The toxicity of these drugs is responsible for the most serious and feared effects of chemotherapy—nausea and vomiting.
As if cancer patients don’t have enough to worry about, the severe and prolonged bouts of vomiting can be so devastating that it is not uncommon for patients to discontinue treatment, even at the expense of their lives. The rate of discontinuation can be as high as 30 percent.
But, now, thanks to a new class of antiemetic drugs called neurokinin-1 (NK1) receptor antagonists, cancer patients will have one less worry. When combined with two other drugs, NK1 antagonists protect most patients —often entirely—from chemotherapy-induced nausea and vomiting (CINV). This is nothing short of incredible.
But first, a little background. The first significant victory in the war against CINV came in 1991, when Glaxo's Zofran was approved by the FDA. The drug provided unprecedented protection against CINV; so much so that most oncologists agreed it revolutionized cancer chemotherapy. Zofran, when combined with dexamethasone, an anti-inflammatory steroid, prevented CINV an unprecedented 75 percent of time, even in patients who were being treated with cisplatin—the worst of the worst emetogenic chemo drugs. Zofran is now on the WHO list of essential medicines. There are now five "setron" drugs (the class name is derived from ondansetron- the generic name for Zofran) that have been approved by the FDA.
Zofran works by blocking the 5-HT3 subtype of serotonin receptors (5-HT is short for 5-hydroxytryptamine, aka serotonin). These receptors are found in the chemoreceptor trigger zone (CTZ) in area postrema of the brain. The evolutionary purpose of these receptors was to respond to certain toxins, most likely from plants, and rid the body of whatever poison was ingested. That may have been very useful when prehistoric man was scavenging for food, but chemo patients have been paying the price for evolution. The CTZs, which are also found in the stomach, do their job too well. Zofran makes them do it less well.
But, there is one significant drawback to Zofran: it doesn't work for long enough. This is because there are two components of CINV: an acute phase (zero-24 hours following chemo), and a delayed phase, which begins between one and five days later, and can last as long as a week. While Zofran works quite well for the former, it does not work well for the latter, so it was not uncommon for chemo patients to benefit in the short term, only to begin vomiting a few days later. This would change profoundly in 2014.
As is the case with a number of other classes of drugs (e.g., HIV medications, antidepressants), combinations of drugs that operate by different mechanism, when combined, can be far superior to either drug alone.
Enter netupitant — the first member of a new class of drugs called neurokinin-1 (NK1) receptor antagonists. NK1 antagonists operate by a different mechanism than that of the setrons. They block the binding of an endogenous neurotransmitter called substance P, to NK1. Since substance P is known to induce the vomiting response when it binds to NK1, blocking this binding should, at least theoretically, prevent CINV in a new way. Would combining the two make a substantial difference? You bet.
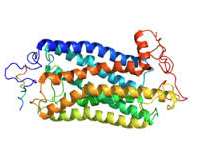
A ribbon diagram of the NK1 receptor
When netupitant was combined with palonosetron, the resulting two-drug combination called Akynzeo, (Merck, FDA approval 2014) when given with dexamethasone, was able to control both acute and delayed-phase CINV. And it did so extremely well:
From the FDA press release: "Results of the first trial showed that 98.5 percent, 90.4 percent and 89.6 percent of Akynzeo-treated participants did not experience any vomiting or require rescue medication for nausea during the acute, delayed and overall phases, respectively (!). In contrast, 89.7 percent, 80.1 percent and 76.5 percent of participants treated with oral palonosetron [plus dexamethasone] did not experience any vomiting or require rescue medication for nausea during the acute, delayed and overall phases, respectively."
(Note: Palonosetron plus dexamethasone does a good job (76-90 percent) in controlling all phases of CINV where Zofran fails. This is because palonosetron is a second generation setron, which was approved in 2003 — 12 years following Zofran, and is much more potent. Palonosetron alone protects about 50 percent of patients from all phases of CINV. Zofran does not). Addition of netupitant and dexamethasone provides 90+ percent protection. This is amazing.
Although, the end results of the research in this area are nothing short of spectacular, getting to this point was anything but easy. Quite the opposite.
Uber-blogger Derek Lowe—the creator of the In the Pipeline blog, which is arguably the most complete and influential site that covers chemistry and pharmaceutical topics, described in 2005 the tortuous path of NK1 receptor antagonists—one that began 80 years ago. Lowe discusses the multiple twists and turns in the development of netupitant. It was a nightmare. Although Merck didn't work on this for 80 years, it must have seemed so to its scientists.
Beginning in the 1980s, the company began the long process of understanding the function of and substance P, as well as the potential uses of a drug that would block its function. At first, it was thought that a substance P blocker would be a good pain killer.
That didn't work out too well: '[T}he outcome from clinical trials [of Merck’s MK-869] has been extremely disappointing with no clear analgesic efficacy being observed in a variety of pain states. This has led the pain community to seriously question the predictability and utility of preclinical pain assays, especially for novel targets.”
The company was not easily discouraged: "MK-869 was the first compound to go into the clinic [as an antidepressant]. And it died there, too. Initial results looked promising – check out this glowing report from 1998. But the next year, it was dropped, after failing to work better than placebo under controlled conditions."
Nightmare, right? Maybe not. Perseverance can pay off: "After much searching around, NK1 antagonism was found to be important enough in nausea and emesis for MK-869 to make it as an adjunct to cancer therapy."
Bingo. A decade later, we now have Akynzeo.
And, on September 4th, things got better. Varubi, a combination of a different setron, and rolapitant, the second member of the NK1 antagonists class, was approved by the FDA. Varubi, which will be sold by Tesaro Inc., a Massachusetts-based oncology specialty biotech, will also be used in combination with dexamethasone. Some scientists give the edge to Varubi because it persists for a very long time in the blood—exactly the property that you would want from a drug that combats delayed phase CINV.
That didn't work out too well: '[T}he outcome from clinical trials [of Merck’s MK-869] has been extremely disappointing with no clear analgesic efficacy being observed in a variety of pain states. This has led the pain community to seriously question the predictability and utility of preclinical pain assays, especially for novel targets.”
The company was not easily discouraged: "MK-869 was the first compound to go into the clinic [as an antidepressant]. And it died there, too. Initial results looked promising – check out this glowing report from 1998. But the next year, it was dropped, after failing to work better than placebo under controlled conditions."
Nightmare, right? Maybe not. Perseverance can pay off: "After much searching around, NK1 antagonism was found to be important enough in nausea and emesis for MK-869 to make it as an adjunct to cancer therapy."
Bingo. A decade later, we now have Akynzeo.
And, on September 4th, things got better. Varubi, a combination of a different setron, and rolapitant, the second member of the NK1 antagonists class, was approved by the FDA. Varubi, which will be sold by Tesaro Inc., a Massachusetts-based oncology specialty biotech, will also be used in combination with dexamethasone. Some scientists give the edge to Varubi because it persists for a very long time in the blood—exactly the property that you would want from a drug that combats delayed phase CINV.
Varubi and Akynzeo will fight it out in the marketplace, but the real winners will be cancer patients, who will benefit from unprecedented control of the dreaded nausea and vomiting that has been poorly controlled in the past. The difference is day and night.
I hope you never need to go through cancer chemotherapy. But, 1 in 2 men, and 1 in 3 women in the United States will develop cancer at some point during their lives. But if you are one of them and require chemo, your life will be immeasurable better than before, because of drugs like these. They are a miracle.
I hope you never need to go through cancer chemotherapy. But, 1 in 2 men, and 1 in 3 women in the United States will develop cancer at some point during their lives. But if you are one of them and require chemo, your life will be immeasurable better than before, because of drugs like these. They are a miracle.





Comments