Bioengineers at the University of California, Berkeley in a new study published in Nature say they have identified two key regulatory pathways that control how well adult stem cells repair and replace damaged tissue. They then tweaked how those stem cells reacted to those biochemical signals to revive the ability of muscle tissue in old mice to repair itself nearly as well as the muscle in the mice's much younger counterparts.
Because the findings relate to adult stem cells that reside in existing tissue, this approach to rejuvenating degenerating muscle eliminates the ethical and medical complications associated with transplanting tissues grown from embryonic stem cells.
The researchers focused on the interplay of two competing molecular pathways that control the stem cells, which sit next to the mature, differentiated cells that make up our working body parts. When the mature cells are damaged or wear out, the stem cells are called into action to begin the process of rebuilding.
Irina Conboy, an assistant professor of bioengineering and an investigator at the Berkeley Stem Cell Center and at the California Institute for Quantitative Biosciences (QB3), led the research team conducting this study. Lead author Morgan Carlson, a recent Ph.D. graduate of Conboy's lab, said, "We are one step closer to having a point of intervention where we can rejuvenate the body's own stem cells so we don't have to suffer from some of the debilitating diseases associated with aging."
"We don't realize it, but as we grow our bodies are constantly being remodeled," said Conboy. "We are constantly falling apart, but we don't notice it much when we're young because we're always being restored. As we age, our stem cells are prevented, through chemical signals, from doing their jobs."
The good news, the researchers said, is that the stem cells in old tissue are still ready and able to perform their regenerative function if they receive the appropriate chemical signals. Studies have shown that when old tissue is placed in an environment of young blood, the stem cells behave as if they are young again.
"Conversely, we have found in a study published last year that even young stem cells rapidly age when placed among blood and tissue from old mice," said Carlson, who will stay on at UC Berkeley to expand his work on stem cell engineering either as a QB3 fellow or a postdoctoral researcher. He will be supervised by Conboy; Tom Alber, professor of biochemistry; and David Schaffer, associate director of the Berkeley Stem Cell Center and professor of chemical engineering.
Adult stem cells have a receptor called Notch that, when activated, tells them that it is time to grow and divide, the researchers said. But stem cells also have a receptor for the protein TGF-beta that sets off a chain reaction activating the molecule pSmad3 and ultimately producing cyclin-dependent kinase (CDK) inhibitors, which regulate the cell's ability to divide.
"Interestingly, activated Notch competes with activated pSmad3 for binding to the regulatory regions of the same CDK inhibitors in the stem cell," said Conboy. "We found that Notch is capable of physically kicking off pSmad3 from the promoters for the CDK inhibitors within the stem cell's nucleus, which tells us that a precise manipulation of the balance of these pathways would allow the ability to control stem cell responses."
Notch and TGF-beta are well known in molecular biology, but Conboy's lab is the first to connect them to the process of aging, and the first to show that they act in opposition to each other within the nucleus of the adult stem cell.
Aging and the inevitable march towards death are, in part, due to the progressive decline of Notch and the increased levels of TGF-beta , producing a one-two punch to the stem cell's capacity to effectively rebuild the body, the researchers said.
"What we discovered is the interplay between two pathways - one an aging pathway, and the other a youthful pathway," said Conboy.
But what would happen if researchers blocked the adult stem cells in old tissues from reacting to those TGF-beta signals? The researchers put that question to the test in a living organism by comparing the muscle regeneration capacity of old, 2-year-old mice, comparable in age to a 75- to 80-year-old human, with that of 2-month-old mice, similar in age to a 20- to 25-year-old human.
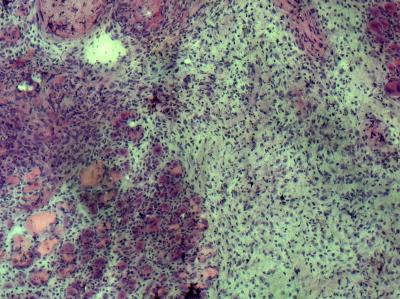
For a group of the old mice, the researchers disabled the "aging pathway" that tells stem cells to stop dividing by using an established method of RNA interference that reduced levels of pSmad3. The researchers then examined the muscle of the different groups of mice one to five days after injury to compare how well the tissue repaired itself.
As expected, the researchers found that muscle tissue in the young mice easily replaced damaged cells with new, healthy cells. In contrast, the areas of damaged muscle in the control group of old mice were characterized by fibroblasts and scar tissue.
However, muscles in the old mice whose stem cell "aging pathway" had been dampened showed levels of cellular regeneration that were comparable to their much younger peers, and that were 3 to 4 times greater than those of the group of "untreated" old mice.
The researchers cautioned that shutting down the TGF-beta/pSmad3 pathway altogether by turning off the gene that controls it could lead to many health problems. The ability to suppress cell division is critical in controlling the development of tumors, for instance.
"When we are young, there is an optimal balance between Notch and TGF-beta," said Conboy. "We need to find out what the levels of these chemicals are in the young so we can calibrate the system when we're older. If we can do that, we could rejuvenate tissue repair for a very long time."
The researchers also warn against interpreting this research as the cure-all for aging.
"We're not at a point where we're ready to inject ourselves with TGF-beta antibodies and call it a day," said Carlson. "There are multiple mechanisms involved in how our body functions. We know that TGF-beta is involved in one aspect of aging, but we don't know where it fits in the global scheme of aging."
In addition to their work on adult stem cells, Carlson and Conboy have also discovered that human embryonic stem cells can actually neutralize the effects of aging. Conboy received funding last year from the California Institute for Regenerative Medicine (CIRM) to pursue this line of research.
Michael Hsu, a former UC Berkeley postdoctoral researcher in bioengineering, also co-authored this paper.
This study was primarily supported by the National Institutes of Health and The Ellison Medical Foundation, with additional funds from a pre-doctoral training grant from CIRM.






Comments